BELMONT, Mich. — September 30, 2025 — AvaSure, the market leader in acute virtual care, proudly announced the recipients of the 9th annual 2025 AvaPrize Awards during the AvaSure Symposium in Charlotte, NC. The AvaPrize honors healthcare organizations and individuals who demonstrate exceptional leadership, innovation, and impact in advancing patient safety and virtual care delivery.
“Each of these winners represents the very best of what is possible in healthcare when vision, leadership, and collaboration come together,” said Adam McMullin, CEO of AvaSure. “We are honored to celebrate their achievements – advancing patient and staff outcomes while reducing costs in meaningful ways, ultimately empowering health systems to better serve their communities.”
2025 AvaPrize Winners
Rookie of the Year Award: Summit Pacific Medical Center
The Acute Care Department at Summit Pacific Medical Center is recognized for their exceptional dedication and resilience during the implementation of their virtual care program. Embracing virtual sitting and new technology required adaptability and teamwork, and the staff demonstrated open-mindedness, perseverance, and commitment to patient safety throughout the transition, leading to a steady increase in utilization and enhanced patient outcomes. In 2025, the team expanded their impact through a collaboration with Mason General Hospital, further expanding virtual care services across institutions.
Breakthrough Innovation Award: Children’s Wisconsin
Children’s Wisconsin is being honored for its visionary approach to virtual care integration. By incorporating ceiling-mounted devices into the design of their new Pediatric Intensive Care Unit (PICU), they established the foundation for a future-ready care model. The phased rollout—from patient visualization, to launching their first virtual sitting program, to now exploring virtual nursing—reflects bold leadership and a commitment to reimagining pediatric care delivery.
Outstanding Operational Excellence Award: Scripps Health
The Scripps Health Central Patient Monitoring Team has been honored with the AvaPrize for their outstanding achievements in advancing virtual care. Through thoughtful expansion, policy refinement, and workflow optimization, the team strengthened cross-department partnerships, reduced reliance on sitters, and created a solid foundation for continued growth. Their collaborative efforts are now shaping the integration of monitoring into new facilities under construction, ensuring lasting impact across the health system.
Centralized Care Champion Award: CommonSpirit Health
CommonSpirit Health seized the opportunity to strengthen its enterprise-wide virtual care strategy and, successfully consolidated operations into a single Phoenix hub command center. This centralized approach embedded analytics into daily practice, enhanced change management, and achieved measurable reductions in falls and sitter cases—all while expanding to new sites. Their work exemplifies how centralization can drive consistency, efficiency, and meaningful patient outcomes across a large health system.
Collaborative Excellence Award: Tucson Medical Center
Tucson Medical Center’s Virtual Nursing Program stands out as a model of multidisciplinary collaboration. From IT teams to bedside nurses, every group contributed to creating a new care delivery model that patients now embrace wholeheartedly. With highly skilled virtual nurses providing patient education and ongoing support, Tucson Medical Center combined the best of traditional nursing care with cutting-edge technology, improving both patient and staff experience.
VA Excellence Award: Tennessee Valley Health System
Tennessee Valley Health System has played a pivotal role in advancing virtual care for veterans in its community. The system strengthened staff training, ensured device readiness, and delivered compassionate patient engagement. These efforts directly prevented falls, increased staff confidence, and established virtual sitters as an integral part of the care team—providing safety, dignity, and reassurance to those who have served.
Virtual Care Superstar Award: Shereia Hill and the Blue Ash Virtual Safety Companion Hub, Bon Secours Mercy Health
As Director of Operations, Shereia Hill transformed the Blue Ash Virtual Safety Companion Hub into a high-performing, connected, and celebrated team. By innovating staffing models, improving handoff processes, and strengthening hospital partnerships, she elevated morale, retention, and patient safety across 19 hospitals. Her leadership during critical transitions—such as relocating 70+ staff to a new facility—exemplifies resilience and vision in virtual care operations.
About the AvaPrize Awards
Launched in 2016, the AvaPrize Awards recognize healthcare leaders and teams who are transforming care delivery with AvaSure’s virtual care platform. Each year, winners are selected for measurable outcomes, culture of collaboration, and innovative approaches to patient safety and clinical excellence.
To learn more about the AvaPrize award, visit https://avasure.com/avaprize/.
About AvaSure
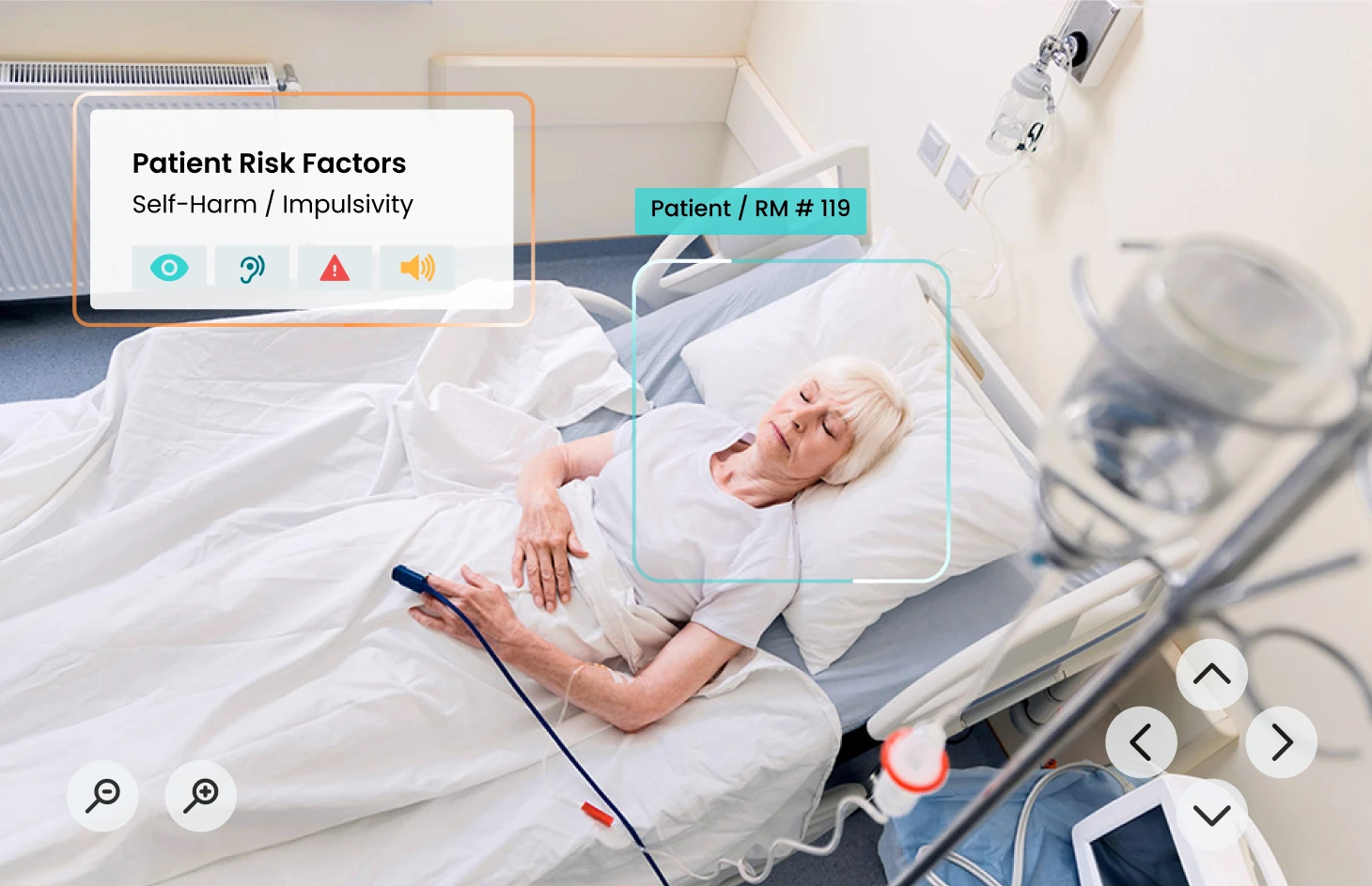
AvaSure® is an intelligent virtual care platform that healthcare providers use to engage with patients, optimize staffing, and seamlessly blend remote and in-person care at scale. The platform deploys AI-powered virtual sitting and virtual nursing solutions, meets the highest enterprise IT standards, and drives measurable outcomes with support from care experts. AvaSure consistently delivers a 6x ROI and has been recognized by KLAS Research as the #1 solution for reducing the cost of care. With a team of 15% nurses, AvaSure is a trusted partner of 1,100+ hospitals with experience in over 5,000 deployments.
AvaSure Media Contact:
Rachel Ford Hutman
301-801-5540
Rachel@fordhutmanmedia.com