In recent memory, no technology has so quickly penetrated the cultural zeitgeist as artificial intelligence (AI). At an ever-increasing pace, AI is being hailed as the hero capable of fixing everything from world hunger to climate change. Companies across the globe are racing to utilize AI to automate, simplify, and rationalize manual tasks across every industry, including healthcare.
At the same time, healthcare has been grappling with tremendous cost pressure & staffing shortages for years. Over the past decade, hospitals have focused on utilizing technology to help drive significant change through:
- Digitization of documentation and communication tools
- Consolidation of health systems in search of economies of scale
- Virtualization of traditional care models to include remote caregivers and stakeholders
In 2020, the COVID-19 pandemic poured gasoline over the fire of those pressures; and hospitals quickly implemented changes to adapt. In many cases, integrated tools are not delivering the simplicity needed; shared data is not delivering the actionable insights that caregivers need; and automation is not allowing care teams to scale that care to an increasing number of patients.
Clearly, there’s no “silver bullet” to remedy all the chaos and pressure. Many key plays need to be run, integrations must deepen, technology needs to be more open to 3rd party access, and virtual experience needs to seamlessly merge with care workflows.
How can AI in healthcare help?
As an industry, we seem to latch on to the hope of the next big thing. Waves of opportunity have come our way with Meaningful Use, Actionable Insights, multi-use case infrastructure like Real-Time Location Systems (RTLS), and more. What does that mean for AI? How can we focus our efforts to soak up as much of the wave as it rolls in?
There are a few key questions we need to answer in determining if utilizing AI in healthcare will truly be the savior it needs, or if it’s just another passing technology fad that won’t deliver on its promises:
What is AI?
What use case examples of AI in healthcare are primed for change?
What risks need to be top of mind when implementing AI in healthcare settings? How can those risks be mitigated?
What is AI?
Let’s tackle what that term, “artificial intelligence,” means. Promising examples of AI in healthcare settings include references to the following technologies:
- Natural Language Processing (NLP) – helps take data from unstructured to structured
- Conversational Bots – virtual agents that manage conversations with patients via text, IM, etc.
- Predictive analytics – mines data to plug into algorithms that project things like patient risk
- Ambient Listening – listens to live audio to turn conversations into notes or identify risks
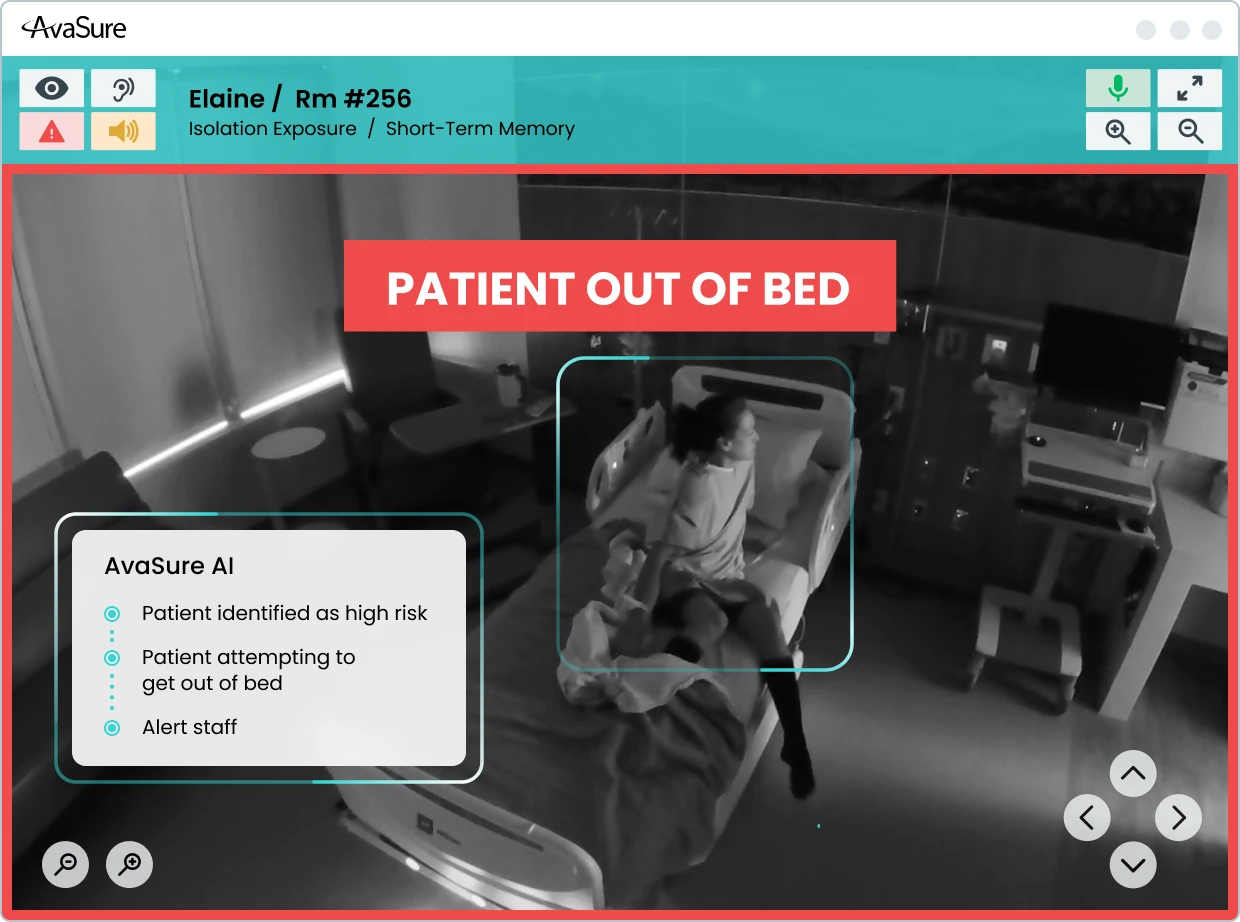
- Computer Vision – watches live video to identify patterns or risks
- Remote Patient Monitoring – uses data from medical devices to anticipate risks or care needs
What use case examples of AI in healthcare are primed for change?
Despite AI’s newfound popularity, some technologies on the list above have been around in healthcare for years. NLP is being used to turn dictated notes into actionable work, like orders, and Predictive Analytics are employed by Populational Health technologies to help target specific populations for focused care based on their risk.
So, if AI in healthcare isn’t anything new, why is it so prevalent in today’s industry discussions? For one, the underlying technology has changed and improved very quickly, making it a more powerful tool. For another, the volume of data needed to improve AI models is becoming more manageable to achieve. As a perfect example, ChatGPT-4 took social media by storm as people began asking for AI to produce legal contracts, bedtime stories for their kids, and essays for homework assignments. Mere weeks later, new forms of this AI were appearing as Chrome extensions that were already better, faster, and stronger than the ones before. The more AI is used, the more valuable it will become because every use provides meaningful learning.
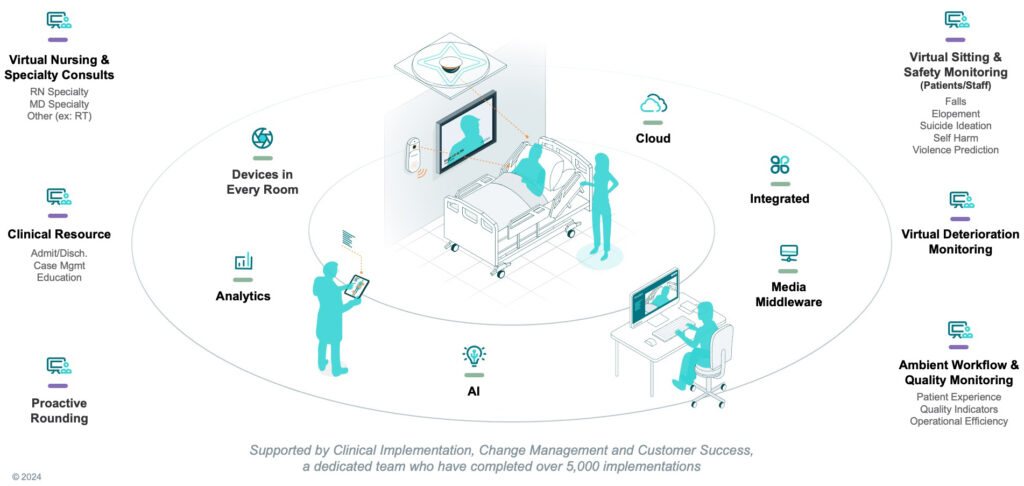
All this progress makes the potential for AI in healthcare more optimistic. Experts agree that, among other things, AI will be key in supporting the push towards more impactful virtual care models. More specifically, this will be achieved through the use of predictive analytics, computer vision, and ambient listening.
During the time that AI entered the conversation, two other important advancements also happened:
- Technology continued to get faster, stronger, and cheaper. Cameras, microphones, speakers, and other equipment necessary to facilitate virtual interactions are now available in more patient rooms than ever before.
- The COVID-19 pandemic opened patients’ and caregivers’ eyes to virtual care, making these interactions more trusted and commonplace.
AI can help turn heavily user dependent devices into seamlessly integrated, clinical workflow-enabling devices. We are entering a moment where the true potential of virtual care is being unlocked, facilitated by the growing prospect of the availability of an AI-enabled virtual care device in every hospital room.
What risks need to be top of mind when implementing AI in healthcare settings?
While one may not be worried about what’s at stake when using AI to help write a bedtime story, the stakes of healthcare are much higher. AI-enabled devices in every hospital room could bring virtual care to life, but there are important questions to consider.
- Are cameras and speakers now the equivalent of a door to the patient room?
- Who decides when the door should be open or closed?
- How do patients, staff, and visitors know that the doors are open, and what does that mean?
- What happens if multiple virtual care team members try to open that door and walk in at the same time?
- Which patients do, or do not, qualify for virtual care models and participation?
- The list goes on….
So, is AI just a short-lived buzzword, or are there clinically relevant use cases that you can take advantage of? Industry experience tells us to avoid getting our hopes up, else our belief in a healthy future might be dashed. We now know that failure is not an option. If we can all see the challenges for what they are and take a mindful approach to what and how we implement, then AI in healthcare may be the ‘silver bullet’ we’ve been promised for years.