Explore their journey of virtual patient monitoring from evaluation to implementation to outcomes, including a significant reduction in falls, zero patient falls with injuries in 2022, and improved staffing efficiencies.
Challenge: Reducing patient falls
CHS, one of the largest provider organizations in the United States, operates across 43 distinct markets in 15 states. Their decade-long commitment to high reliability, safety, and harm reduction aligned perfectly with the need to reduce falls during the pandemic in 2021. Hospitals across the nation have been grappling with staffing shortages, leading to nurse burnout and a rise in adverse patient events. As the personnel issue worsened, many healthcare systems asked: How can hospitals create a care system that reduces the need for 1:1 patient sitters while allowing nurses to focus on critical patient care?
Evaluating solutions: Evidence and scalability
In their quest for the right solution, CHS employs a rigorous evaluation process. Their primary criteria encompass two crucial elements: evidence-based effectiveness and scalability. First and foremost, CHS seeks evidence-backed solutions, emphasizing clinical outcomes and operational impacts. This commitment to data-driven decision-making ensures that any chosen solution delivers tangible benefits across both patient care and operational efficiency.
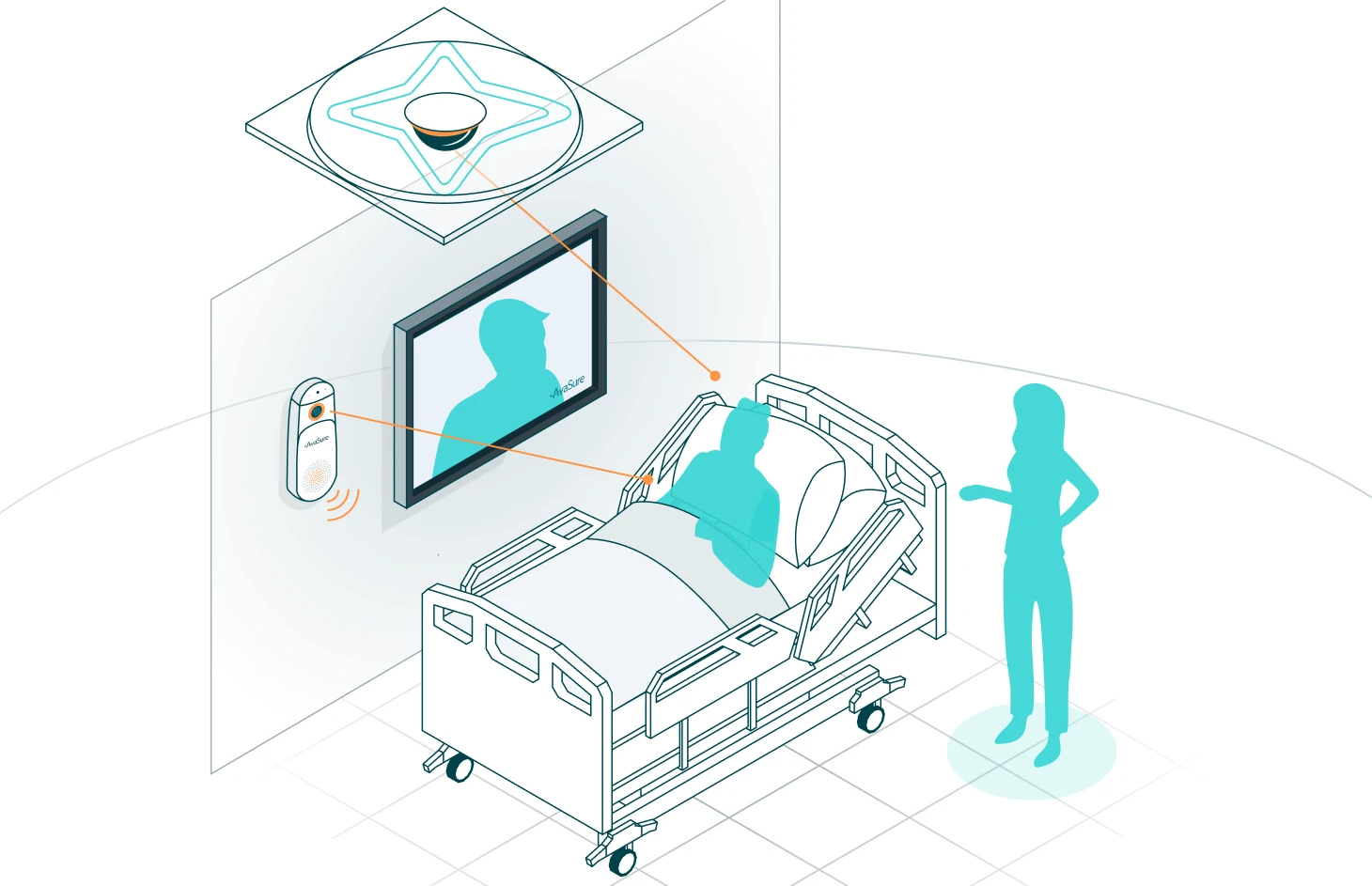
The second key criterion is scalability. Given CHS’s size, the ability to initially implement a solution at a few select hospitals and then scale it elsewhere across the organization is paramount. In this regard, AvaSure’s TeleSitter solution met these criteria for virtual patient monitoring, making it a natural choice to address their needs.
Phase 1 deployment: Keys to success
CHS’s journey with the AvaSure TeleSitter solution commenced with a pilot deployment at three hospitals and then scaled to 17. This pivotal phase yielded notable success, attributed to several critical factors:
- Intentionality: The deployment of virtual patient monitoring was marked by a deliberate and well-thought-out strategy. Every step was carefully considered, from initial planning to execution, ensuring a seamless integration of the TeleSitter solution into their healthcare ecosystem.
- Metrics that matter: A key driver of success was CHS’s dedication to data-driven decision-making. They recognized the importance of collecting precise and relevant data to assess the impact of the TeleSitter solution accurately. This commitment to meaningful metrics allowed them to track progress, identify areas for improvement, and ultimately optimize patient care outcomes.
- Leadership and oversight: Strong leadership and dedicated oversight were pivotal throughout the deployment process. Key leaders within CHS played a central role in driving the virtual patient monitoring initiative forward. Their unwavering commitment and guidance ensured that the program remained aligned with the organization’s broader goals and objectives.
- Buy-in and Teamwork: CHS understood that achieving the desired results required a collaborative effort. Encouraging buy-in and utilization among staff was essential. Through effective communication, collaboration, and trust, the healthcare team worked together to maximize the benefits of the TeleSitter solution. It became a team effort, with everyone playing a crucial role in its success.
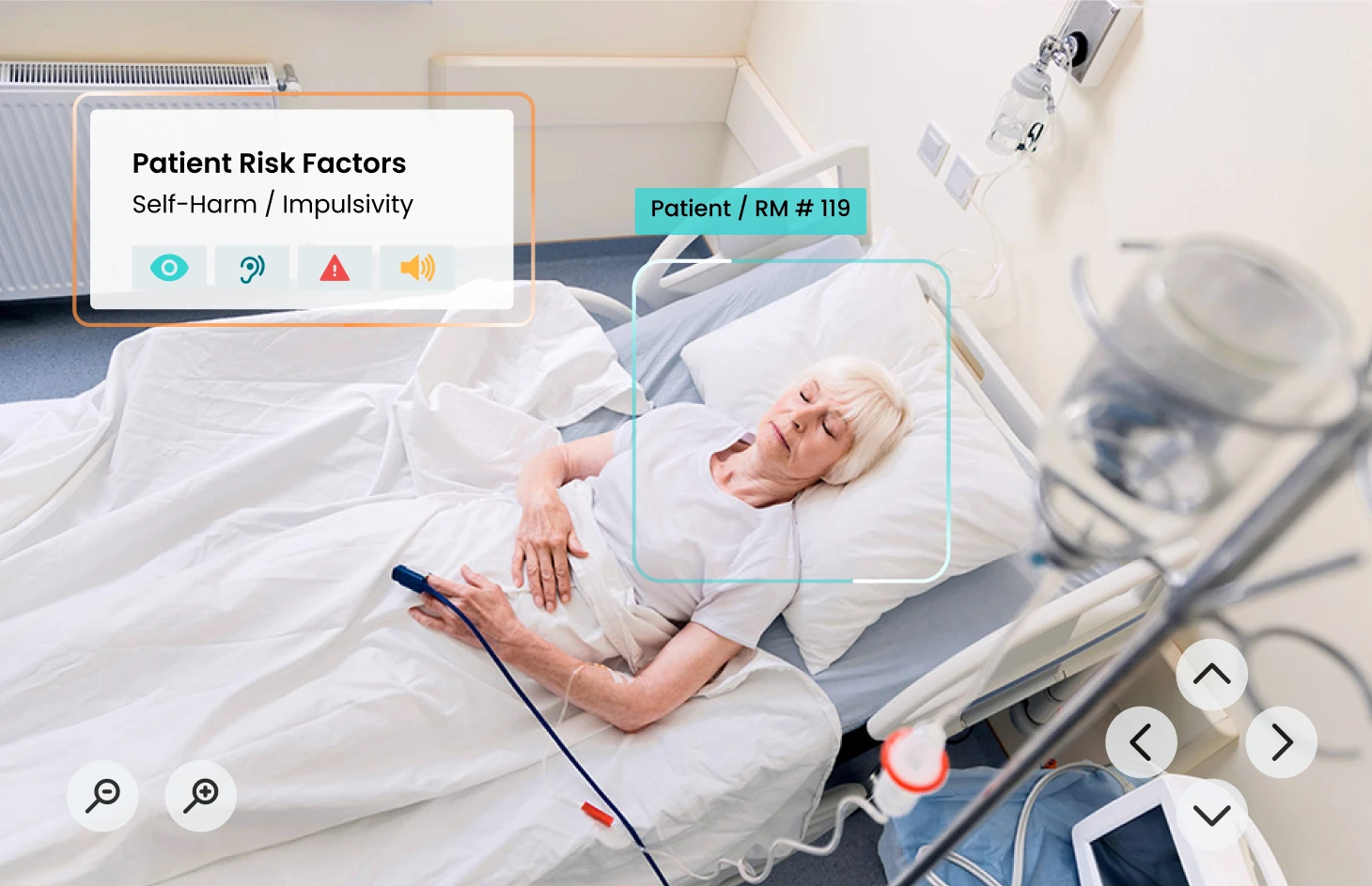
- Strategic Patient Selection: CHS recognized the importance of strategic patient selection in applying the technology where it would be most effective. Careful consideration was given to identifying patients who would benefit most from the TeleSitter solution, further optimizing its impact on patient safety and care quality.
This comprehensive approach to the Phase 1 deployment set the stage for CHS’s journey implementing virtual patient monitoring, paving the way for positive clinical and operational results.
Outcomes: Reduction in falls and positive operational and financial impact
Following the completion of the pilot program, CHS embarked on a thorough analysis, which unveiled some significant outcomes.
- A Meaningful decrease in falls: While CHS has worked effectively to reduce falls for years, implementation of the TeleSitter solution led to an even greater reduction in falls, including a 76% reduction in one hospital.
- Zero patient falls with injuries in 2022: In 2022, CHS reported zero patient falls with injuries at facilities using virtual patient monitoring. This milestone reflects a profound commitment to patient safety.
- Savings through injury avoidance: The solution translated into meaningful savings through the avoidance of costs related to patient injuries. In an environment where litigation looms, AvaSure can help mitigate potential liability claims when it comes to falls with injury.
- Staffing dfficiencies of 16 to 1: The introduction of virtual sitters had a strong effect on staffing efficiency. With each virtual sitter capable of monitoring up to 16 patients simultaneously, CHS achieved staffing efficiencies of 16 to 1. This efficiency not only optimized staffing allocation but also enabled caregivers in CHS hospitals to work at the top of their licenses and provide more attentive care to a broader patient population.
These outcomes are a testament to CHS’s commitment to excellence, safety, and innovation. AvaSure delivered quantifiable operational benefit and helped reinforce the high standard of patient care and safety across CHS.
Quality and patient care lead to next steps
Today, CHS is poised to expand virtual patient monitoring services. With 87 devices currently in place, CHS plans to add 78 more across 12 more hospitals by the end of 2023.
CHS’s innovative approach helps ensure that more patients are kept safe, more healthcare professionals are supported, and the future of healthcare is brighter than ever.
Watch the webinar replay to hear firsthand from CHS about how they expanded their virtual patient monitoring program to enhance patient safety and optimize resource utilization.
Today, CHS is poised to expand virtual patient monitoring services. With 87 devices currently in place, CHS plans to add 78 more across 12 more hospitals by the end of 2023.