By Lisbeth Votruba, MSN, RN
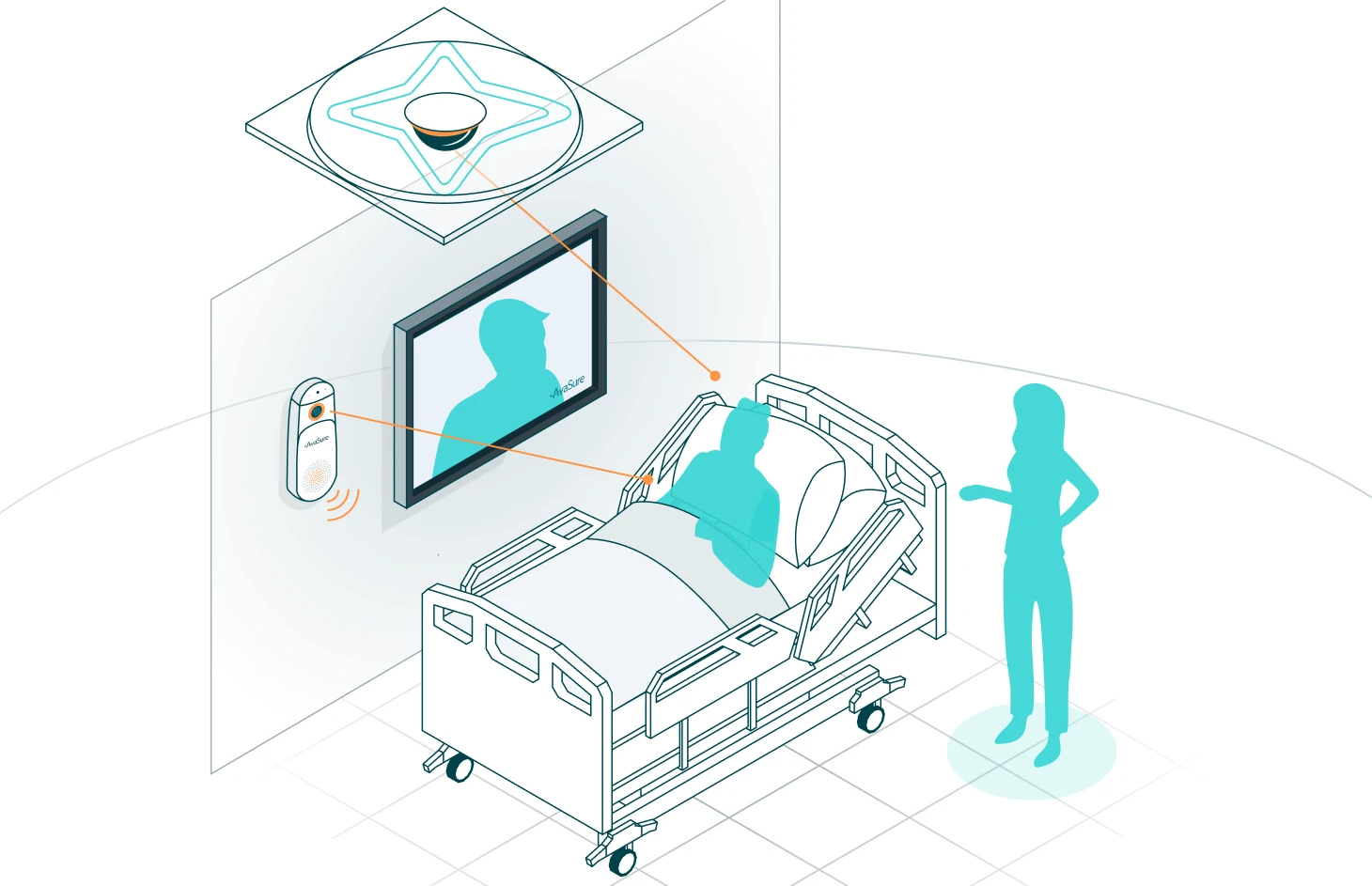
Over the past year, there have been numerous publications, pilots, and discussions on virtual care. Many organizations are planning for a future where virtual team members are seamlessly integrated into care teams, where a device exists in every room enabling episodic and continuous video visits and where technology helps to augment nursing staff. However, amongst these conversations there is little clarity or direction on how to get there. Throughout AvaSure’s 5,000+ deployments at over 1,100 customer sites, we have collected best practices on implementing virtual care programs that deliver real results and outcomes. We employ clinicians at all levels of our organization who are engaged in forums across the country, led by AONL, AMSN, ATA, and others, on the creation of these virtual teams. Based on our work with early adopters and these industry experts, we have designed a prescriptive path to achieving the future of a fully integrated virtual care facility.
AvaSure’s Intelligent Virtual Care Adoption Model
Defining the 5 stages
The AvaSure Intelligent Virtual Care Adoption Model consists of five progressive stages, each of which builds on the foundation of the prior stage to financially fuel the next step, generating real patient outcomes at every stage.
Stage 1: Implement virtual sitting
The virtual care adoption model begins with implementing virtual sitters, who are trained, unlicensed personnel who use video and audio connections to watch over patients aiming to improve overall safety. The primary goals of this stage are to enhance patient safety while replacing up to 75% of one-to-one sitters for at-risk patients with virtual sitters. The clinical evidence demonstrating virtual sitting is superior to in-person sitters for preventing falls is irrefutable. The return on investment is robust, stemming from increased staffing efficiency at a ratio of 1-to-12 instead of 1-to-1, along with substantial cost savings resulting from reduced falls. These savings can be directed towards improving the hospital’s bottom line or reinvested to support subsequent phases of the adoption model.
Stage 2: Optimize virtual sitting
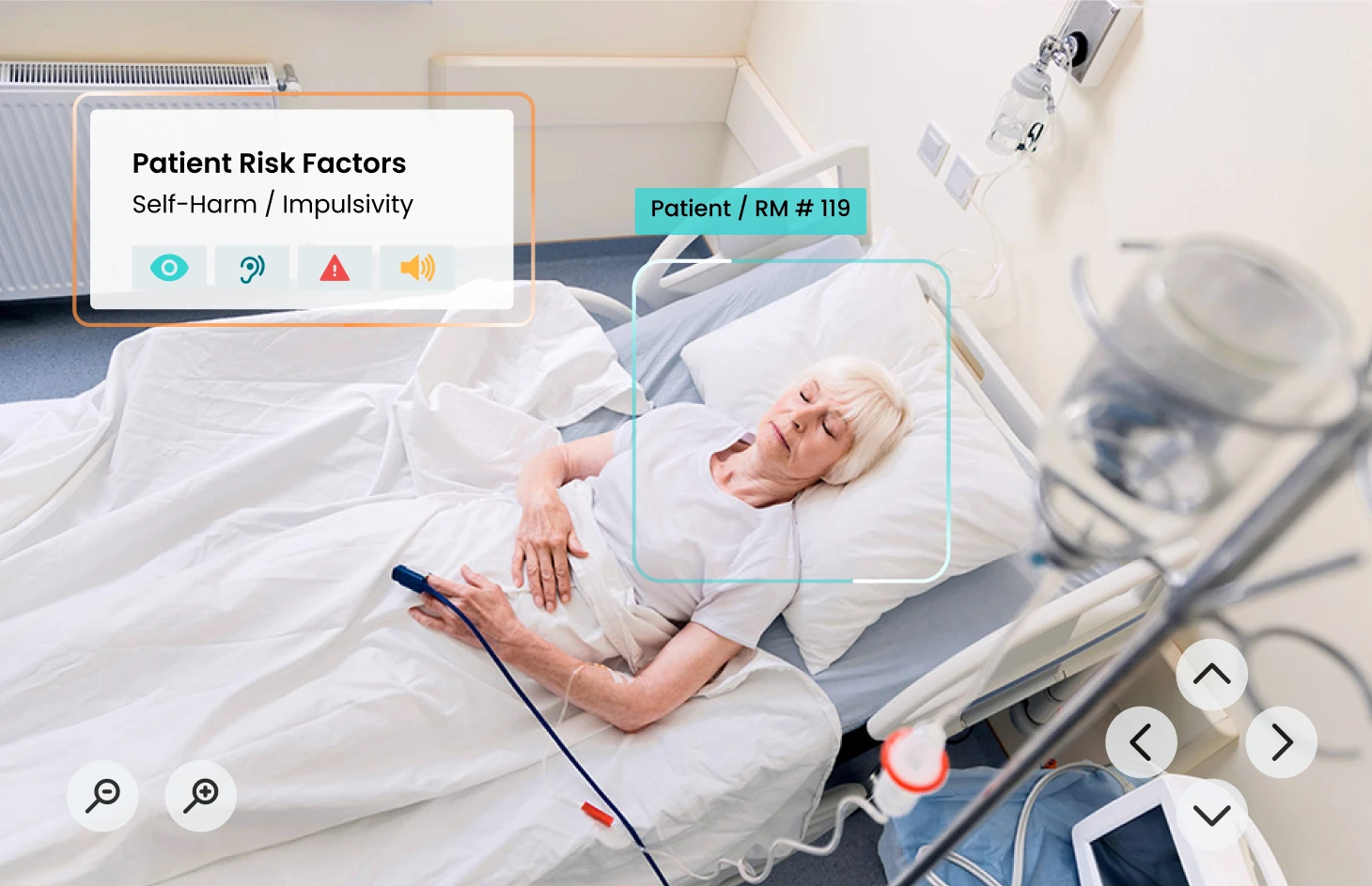
In the second stage, hospitals can look to optimize their virtual sitting program through expansion to other use cases and care units. Beyond falls, other established use cases include elopement, substance use withdrawal, low/moderate suicide risk, pediatrics, workplace violence prevention, and more. The staffing efficiency of virtual sitting allows hospitals to expand the reach of monitoring from what is feasible to cover with 1-to-1 staffing and cover additional use cases covering up to 20% and 25% of patient beds.
Upon recognizing the success and cost savings of virtual sitting, many organizations choose to centralize their monitoring across the health system leading to further efficiencies of scale. For example, Trinity Health implemented AvaSure system-wide, covering 25 states in just nine months. Patient monitoring is conducted from two central “super hub” locations. At this scale, the health system was able to provide 1.8 million hours of virtual sitting at 85% less cost ($24 million) in 2021.
Finally, integrating artificial intelligence (AI) to supplement virtual staff assists in alleviating the cognitive burden on virtual care staff. This improvement not only automatically alerts staff to potential risks of adverse events but also contributes to better outcomes.
Stage 3: Launch virtual nursing with return-on-investment from virtual sitting
Upon realizing substantial labor savings and cost avoidance through enhanced patient safety, these funds can be employed to initiate a virtual nursing program utilizing the same devices and platform.
A fundamental goal of any virtual nursing program is to allow nurses to work at the top of their license. This is not possible when there is a shortage of unlicensed personnel. Having freed up personnel from 1-to-1 sitting tasks, they are better able to support bedside RNs in a model of care that virtual nursing can also support. Many facilities choose to start with admission and discharge support, where a virtual nurse helps with the documentation and administrative tasks, supporting the bedside RN. However, based on organizational goals – there are a multitude of use cases virtual nursing can pilot with.
Holzer Health System, a two-hospital system in Ohio, is currently in stage 3 with an inpatient virtual care program. The health system implemented the program to address challenges associated with patient safety as well as issues with patient access to specialty care. The hospital installed a total of 16 monitoring devices, providing both virtual sitting and virtual specialty care from a central hub. “I am the only certified wound and ostomy nurse for inpatient facilities at Gallipolis and Jackson.This has provided a way for me to do video consults with the Jackson facility, which saves precious time as well as mileage,” said Natalie Gardner, BSN, RN, CWON, CFCS.
Stage 4: Optimize virtual nursing
After a virtual nursing pilot demonstrates its efficacy in enhancing specific areas such as nurse satisfaction and retention, expediting patient flow, or reducing adverse events, then it’s time to scale up.
One example of an AvaSure customer that has optimized its virtual nursing program is UCHealth, a nonprofit healthcare organization based in Colorado that consists of 13 hospitals and 2,000 inpatient beds across the state.
Three years following the success of its virtual sitting program in enhancing patient care, UCHealth broadened its virtual care capabilities by including a virtual nursing program. This program, facilitated by experienced nurses, assists clinicians in promptly identifying hospitalized patients exhibiting signs of deterioration. This early detection enables clinicians to administer timely treatment, ultimately leading to improved patient outcomes.
UCHealth has 693 AvaSure devices (both mobile and fixed room devices) installed across the health system. Senior, expert nurses at the Virtual Health Center can visualize ICU patients across the health system as well as patients outside ICU who have a rapid response call activated. The health system utilizes AI deterioration algorithms to proactively intervene. This has led to improved sepsis detection, and decreased code blues, but most importantly, Dr. Hemali Patel, Associate Chief Medical Officer, explained the virtual care team has helped save the lives of 786 patients together with the frontline staff.
Stage 5: System-wide adoption
The culmination of intelligent virtual care adoption will include a device in every room and have virtual team members seamlessly integrated into every care team. Technology is being used to provide exceptional experiences for both the patient and caregivers, helping to continuously improve outcomes, fully optimize the labor force, keep labor costs manageable, and bring joy back to caregiving.
The Key to Success: The AvaSure Advantage
Faced with high labor costs and a dwindling supply of workers, many hospitals across the nation are in various stages of virtual nursing adoption – a number that is sure to rise as health systems’ operating challenges persist. As they do, the primary use case for virtual nursing today – rounding, admissions and discharge, patient education, documentation support – will be joined by other applications of this emerging technology. However, success may seem unattainable without a coherent business case, buy in of clinical and IT teams, and achievable KPIs.
AvaSure has the expertise to guide hospitals through their virtual care adoption journeys. We have a platform with the necessary technology to support a multitude of use cases, but more importantly we have the clinical expertise to help develop your program from the ground up. From policy and procedure development, workflow design and change management support, our people will be the difference in making your program a success. Backed with data and insights, we can help hospitals stair step your way to the deployment of an intelligent virtual care platform, helping you step into a future where cutting-edge technology and compassionate care converge.