
Last week AvaSure hosted our 1st Annual Digital Summit: Start, Scale & Succeed with Virtual Sitting. During this one-day educational event, we featured over 10 current AvaSure customers to share their best practices & learnings from deploying virtual sitting programs. Read on to hear how they were able to improve outcomes, optimize their labor force and protect staff all while helping to reduce costs.
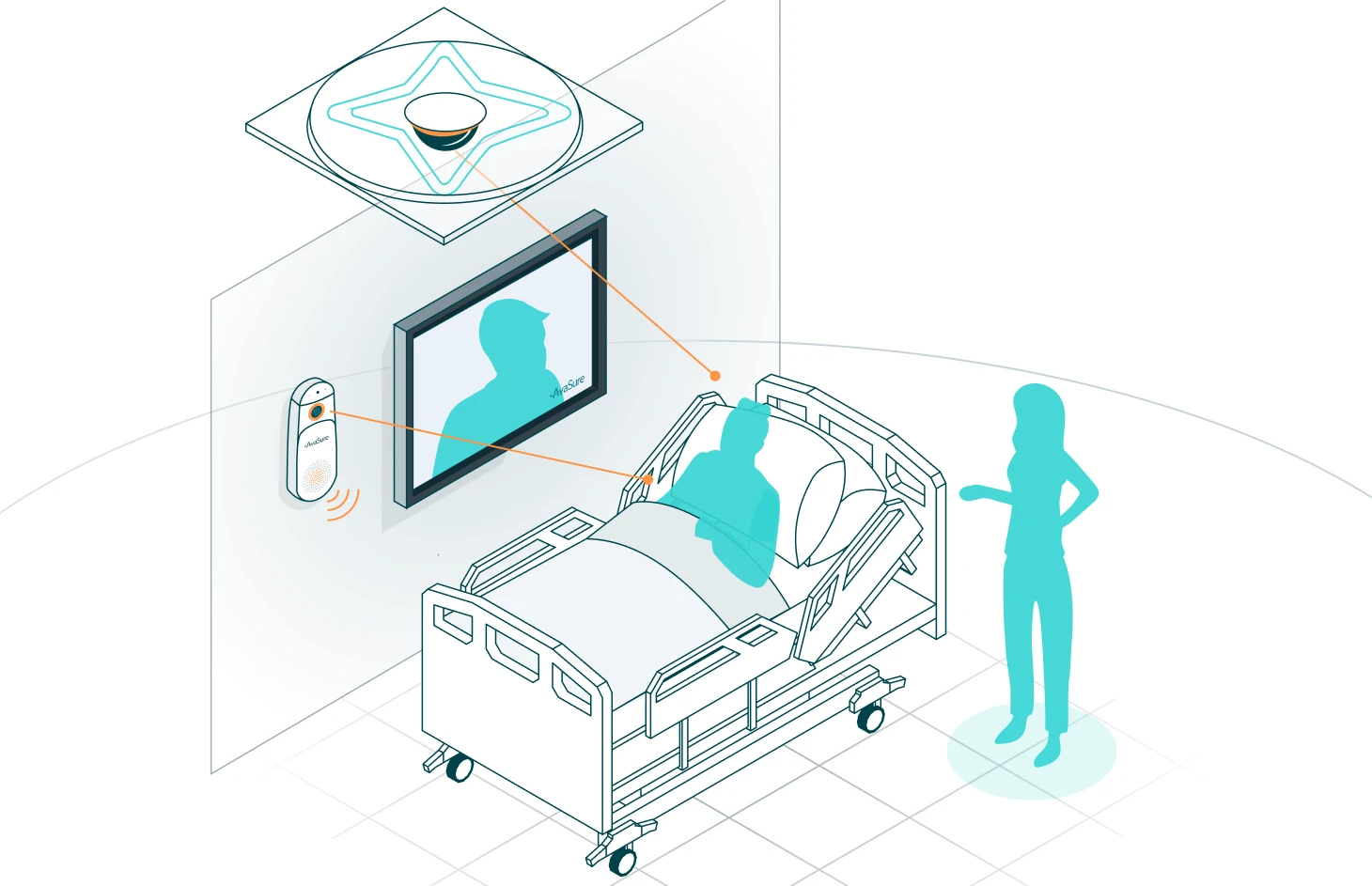
There were so many exceptional discussions centered around today’s challenges – staffing being front and center. We know that hospitals across the U.S. are struggling to find enough nurses and support staff to run efficiently, so technology is helping to bridge the gap. With the AvaSure TeleSitter® Solution, hospitals are replacing the need for traditional 1:1 sitters by using Virtual Safety Attendants (VSAs) to monitor up to 12 patients remotely while reducing adverse events. Seem too good to be true? The results just may be.
How Valley Health Reduced the Use of 1:1 Sitters While Decreasing Falls
Valley Health System shared their story of starting a TeleSitter program four years ago that has gone on to help:
- Reduce falls with injury by 50%
- Save over $1 million dollars from combined fall reduction and sitter cost reduction
- Achieve an 80% device utilization across the system
When discussing why they chose to work with AvaSure, they said, “We wanted to work with the experts to show us how this has worked at other organizations. Other organizations have made mistakes, had those mistakes corrected and so we are the beneficiaries of that. We wanted to focus on what we are good at. What we aren’t good at is setting up our own sitter program. But, what we are good at is knowing our needs, selecting the best partner out there and picking someone who could address our needs today & help us go beyond that in the future.” AvaSure has helped over 1,000 customers just like Valley Health start their programs and we have the clinical expertise to help make it as turnkey as possible for your staff.
Use Cases for TeleSitter solutions extend beyond just falls
Success of virtual sitting extends beyond just the acute care setting, Gaylord Specialty Healthcare gave a sneak preview of yet-to-be published results of how AvaSure helped optimize their LTACH program.
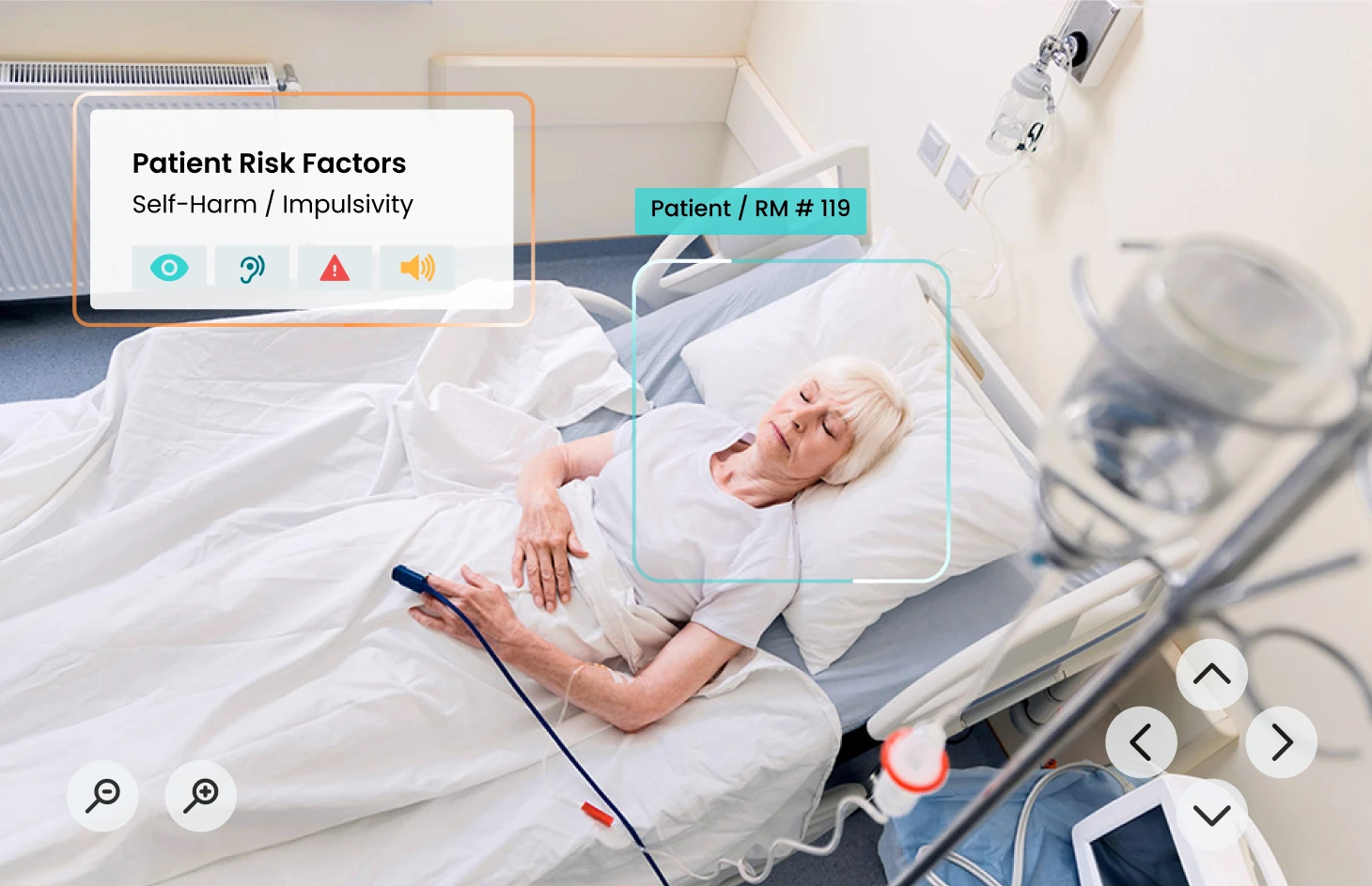
While virtual sitting programs may be best known for helping reduce falls, their use extends far beyond that one use case. We heard from Rachel Krajnovich, MSN, RN-BC, Director of Clinical Operations at HCA Kingwood on utilizing virtual monitoring for suicide risk & behavioral health patients.
- Suicide is the 12th leading cause of death in the U.S. across all age groups and the number of patients requiring suicide monitoring in acute care has increased 165% since 2019
- 45% of hospitals that utilize AvaSure have monitored over 75,000 suicide risk patients across 45 states
This lesser-known use case can be extremely effective in helping to monitor low and moderate suicide risk patients, and is proven to be equally effective to in-person sitters for this population(1). These customers shared best practices regarding how they evaluate patients to be placed in the program, how they helped to get physicians and staff on board with utilizing virtual monitoring for this high-risk population and how it has helped them extend access of needed yet scarce mental health resources in ERs today.
Expanding to other use cases is just one example of scaling your program, you can also help to extend the reach of your program across various facilities in your system, helping you to achieve greater scale and efficiency. Providence Oregon Region shared how they built a ‘hub and spoke’ model – which involves having devices across multiple facilities with monitor staff at one, centralized hub watching patients across the system. This can help create a highly effective staff that is able to protect patients across the system and optimize your device utilization. Hear how they were able to achieve an average stat alarm response time of 12-15 seconds, well below the national average of 17 seconds.
Virtual Safety Attendants are Key to Program Success
As always, one of our most popular sessions was best practices from Virtual Safety Attendants – sharing how they’ve built teams of heroes that work 24/7 to connect with patients, keep them safe, keep them calm & help assist them on their recovery journey. We heard from a VSA, Tom Dezell from Froedtert, who shared when thinking back on advice he’d give himself on his first day:
“That I cannot let my fear of something happening to the patient interfere with my taking care of the patient. In other words, I can’t respond out of fear, I have to respond out of patient advocacy and confidence.”
His demonstrated commitment to his patients brought emotions to all who listened as he spoke so passionately and eloquently about the time he spends helping patients.
What Does the Future of Virtual Care Look Like?
We closed the day with Claire Zangerle, DNP, MBA, RN, NEA-BC, FAONL, FAAN, Nurse Executive with CMZ Strategies, LLC discussing the future of virtual care with AvaSure Chief Clinical Officer, Lisbeth Votruba, MSN, RN. In discussing her hopes for the future of nursing in this new virtual care environment she said,
“It’s our time as nurses to step up and make sure we’re listened to. We have to tell people how great it is to be a nurse and what it means to be a nurse. We’re in danger of people saying that the job is too hard to do. Everyone wants to work remote now, you can’t be hands on and work remote. You have to promote the value of human interaction, it’s so important. We know we don’t have enough staff and enough people to do human interaction whether it’s in a hospital, ASC, community health center, we know we don’t have enough people. We need to meet patients where they are, and we need to think of new ways to meet patients. We aren’t thinking about this because we don’t have enough staff, it’s also because that’s what patients want. We are looking at ways to make sure they get what they want.”
Nursing has always been and will always be an essential and noble profession that relies on hands-on patient care, clinical expertise & empathizers who care deeply about the lives of their patients. AvaSure believes that nurses should always be central to care, which is why we featured nurses throughout our summit – as moderators, hosts & panelists to demonstrate the vital role they play in the shifting care model moving forward.
We look forward to sharing more insights, recaps and full session replays of Digital Summit for those who have missed it.
1 Kroll, D. S. et al., (2020). Virtual monitoring of suicide risk in the general hospital and emergency department. General hospital psychiatry, 63, 33–38. https://doi.org/10.1016/j.genhosppsych.2019.01.002