Industry experts, healthcare leaders & the market have all agreed – virtual nursing is here to stay. In a 2024 study, 74% of hospital leaders reported that virtual nursing will become integral to care delivery models in acute inpatient care —up from 66% in 20231. However, only 10% of hospital leaders have reached a phase where virtual care is a standard part of care delivery, and nearly 30% of hospitals have no virtual care workflows at all1.
Why the gap?
Pilot or partial deployments of virtual nursing are where most institutions are getting stuck!

How can we break through perpetual pilots and scale virtual nursing to be a standard part of care delivery?
Let’s ask the experts.
AvaSure, a leading provider of Intelligent Virtual Care Platforms, consulted with two leading healthcare institutions that have successfully moved beyond the pilot phase and fully integrated virtual nursing into their daily patient care. Together, they explored how these organizations made the transition and shared valuable insights and advice for other institutions just beginning their virtual nursing journey.
UCHealth, a nationally recognized healthcare system with $7.5 billion in operating revenue and over 33,000 employees, operates 14 Colorado hospitals, providing more than 2,500 inpatient beds, and over 200 clinics across Colorado, southern Wyoming, and western Nebraska. Their 2016 Virtual Health Center significantly enhances patient care through virtual deterioration monitoring, TeleICU, centralized telemetry, virtual admission & discharge support, virtual sitting, virtual consults & more. This Virtual Health Center has touched over 2.3 million patient lives, achieving remarkable outcomes like reducing code blue rates by up to 40%, increasing rapid response rates and improving patient safety through virtual sitting, yielding nearly $9 million in 1:1 sitter cost savings. To support these expanded use-cases and future-proof the patient room for a hybrid patient care model, UCHealth implemented a ‘camera-in-every-room’ philosophy.
Amy Hassell, MSN, BSN, RN, CNO of Virtual Health Center, UCHealth
Tamera Dunseth Rosenbaum, DNP, RN, NE-BC, System CNO of UCHealth

As New Jersey’s largest and most comprehensive not-for-profit healthcare network, Hackensack Meridian Health (HMH) delivers a full spectrum of medical services, innovative research, and life-enhancing care through its 18 hospitals, 36,000+ team members, 7,000 physicians, and 500+ patient care sites. HMH kicked off their virtual nursing journey in 2022 with the goal of improving outcomes and patient/provider satisfaction. With a virtual nursing pilot focused on virtual admission & discharge support, they successfully removed time-consuming task-based work from bedside teams. Following a year of successful implementation, the results prompted hospital leadership to expand the program across four hospitals.
- 11.6% reduction in length of stay
- 65% reduction in RN traveler hours and 26% reduction in RN overtime hours
- 0.68% reduction in readmission rates
Marie Foley-Danecker, DNP, RN, CCRN, NE-BE, Vice President & Chief Nursing Office of Hackensack Meridian Health
Pilot sticking point: Lack of organizational alignment on program goal requires vision & change management
Lesson One: It requires both leadership support and buy-in from frontline staff to be successful.
The true blending of virtual and in-person clinical workflows is a technology investment, a change in nursing practice and a change in patient care – so “don’t underestimate the amount of cross-functional alignment it takes to get to one platform, one operating strategy across the network – it takes a village,” said Marie Foley-Danecker. HMH has 5 distinct project teams that stood up to help scale their pilot across the system:
- Tech Build Team (Both Network and Site Level) – make decisions around hardware, software, server, infrastructure, hosting and more – ensuring the system has not just the right technology, but the support infrastructure needed to support ongoing virtual care.
- Clinical Workflow Team – help to ensure that bedside workflows are standardized and the virtual workflows fit seamlessly into them. If you don’t start with standard work at the bedside, it will be nearly impossible to add a virtual care workflow.
- Nursing Operations Team – help manage staffing, define roles & responsibilities between team members and drive collaboration
- Education Team – ensure the internal education of facility teams, as well as patients & family members so that they understand the role of the virtual care team members in their visit
- Communications Team – tackle marketing and promotion of the program externally, helping to improve the hospital’s reputation as a cutting-edge, patient-experience oriented site of care. Robust virtual care programs can also act as great recruitment tools for future nurses who want to work at systems investing in the latest technology.
Lesson Two: Prepare for and be willing to adapt quickly.
“Be nimble and understand that you might not get it right, right out of the gate. That’s why having a governance structure (like the teams at HMH or a steering committee approach at UCHealth) that can be quick to identify issues and change processes is really important” said Tamera Dunseth Rosenbaum. It’s essential to remember the primary reason why you’re doing this – to provide support to your bedside teams. So, listen to them! Be sure to take in their ideas of what may help and lean into those ideas. Example: HMH, at the suggestion of front-line teams and following suit of many facilities, chose to start with admission & discharge as their first virtual nursing use case. Bedside team members see a lot of value in the ability to offload task-based, administrative work to virtual teams in order to give them more time for hands-on patient care. Furthermore, virtual care team members who are focused specifically on admission & discharge – or other task-based nursing work – can be hyper focused, resulting in spending more time connecting with the patient and often seeing better results. A true win/win! Similarly, UCHealth chose to utilize the virtual nurse answer and triage call lights as a part of their first use case. However, it quickly became apparent that this was adding burden to the bedside with unnecessary steps and communication overload. They took note, quickly changed course, and have since seen greater success. This willingness to adapt & change will be critical to the success of any virtual care program – and to winning the support of your team.
Lesson Three: Build grassroots support.
The bedside team is critical for program success, so giving them a voice is essential. If you don’t know where to start, listen to your front-line nurses – and think about what would make their lives easier. Selecting a first use case that directly benefits them will help with long-term program success. As you get to more complex use cases, like TeleICU, virtual deterioration monitoring, TeleStroke and more, trust between virtual and bedside teams will be vital. You can build this trust through making front-line nurses feel a part of the implementation, ideation, and ongoing governance of the virtual nursing program.
Pilot sticking point: staffing the program
Many facilities are already struggling with the chronic staffing shortage, so how do you find the staff for a virtual nursing program? There are two main paths – utilize your existing talent pool to fill virtual roles or work with a staffing partner who can help provide the adequate staff for your program. Let’s discuss each model & the pros/cons of each.
Utilizing your existing talent pool
Tips & things to consider:
- Keep job descriptions consistent between on-site and virtual: This allows for flexibility for floating or job sharing between bedside and virtual roles, without creating unnecessary HR hurdles. Also, offering a virtual shift can be a nice benefit to bedside team members – facilities use this to reward seniority, help prevent burnout and improve staff satisfaction.
- Think outside your geography: The nursing shortage is more acute in certain regions. For example, HMH, located in New Jersey, knew that finding nurses in this expensive, metropolitan area would potentially prevent getting their program off the ground. In this instance, working with a partner based out of Tennessee with a richer talent pool, like Equum Medical, made sense for avoiding staffing restraints that would prevent them from getting their program started.
- Evaluate the experience level of your current staff: If your facility is predominantly novice nurses, you’ll need your most experienced nurses at the bedside to make virtual care a success. Pulling these nurses into virtual roles could potentially increase travel nurse/overtime use, offsetting potential program ROI. In these cases, outsourcing with a staffing partner may be a better fit for your institution.
Working with a virtual staffing provider
Tips & things to consider:
- Speed to go-live: Outsourcing to a trusted provider of virtual nurse staffing may allow you to get started quicker, as they have teams ready to deploy immediately. You can always consider moving things in-house overtime once your program is scaled.
- Add more use cases with supplemental staffing: Staffing doesn’t need to be all in-house or all partners! You can take a use case driven approach and use a staffing partner to fill gaps in your team’s experience. Outsource staffing for more complex use cases, like virtual patient deterioration or TeleICU.
Important insight: Marie Foley-Danecker said, “trust is earned—whether you choose to use a partner or have your own staff on the virtual team, the beside team will take time to trust them. Don’t assume that trust will be built immediately just because you use your own staff, or assume trust can’t be built if you outsource.”
Pilot sticking point: funding the program
One of the most talked about reasons for the lack of virtual nursing adoption is the funding. Like many things, leaders struggle to build the business case to pay for it. Some have a misconception that only affluent health systems, or those with a highly favorable payor mix, can afford it. However, HMH and UCHealth both have a challenging payor mix across their system and had to work hard to validate the business case to leadership. Some of their lessons learned include:
Allocating virtual nurse resources to each department.
UCHealth accomplishes this by allocating a small unit of service bump to each department that utilizes the virtual resource. At the care unit level, it can be as small as 0.1 – 0.2 hours per patient day, but UCHealth recommends this path for a few reasons:
- Encourages use of the virtual team – if the department is “paying for it anyways”, they’re more likely to utilize the virtual team, helping to improve program utilization.
- Helps to spread the cost and avoid constant justification to hospital leadership – When the entire virtual care program is consolidated under a single budget, it becomes a frequent target for scrutiny during budget reviews. Spreading the allocation makes it less likely to face ongoing questioning or review.
- Tip: Be sure to have the virtual resource as a separate line item on each nurse manager’s budget to remind them that this is the FTE for the virtual team support. Otherwise, they may hire up to that amount, and the program will be over budget.
- Hits budgetary targets – With turnover and vacancy rates most departments can still hit their budgetary targets with this allocation.
Labor savings from virtual sitting can help fund investment in devices for other use cases – like virtual nursing.
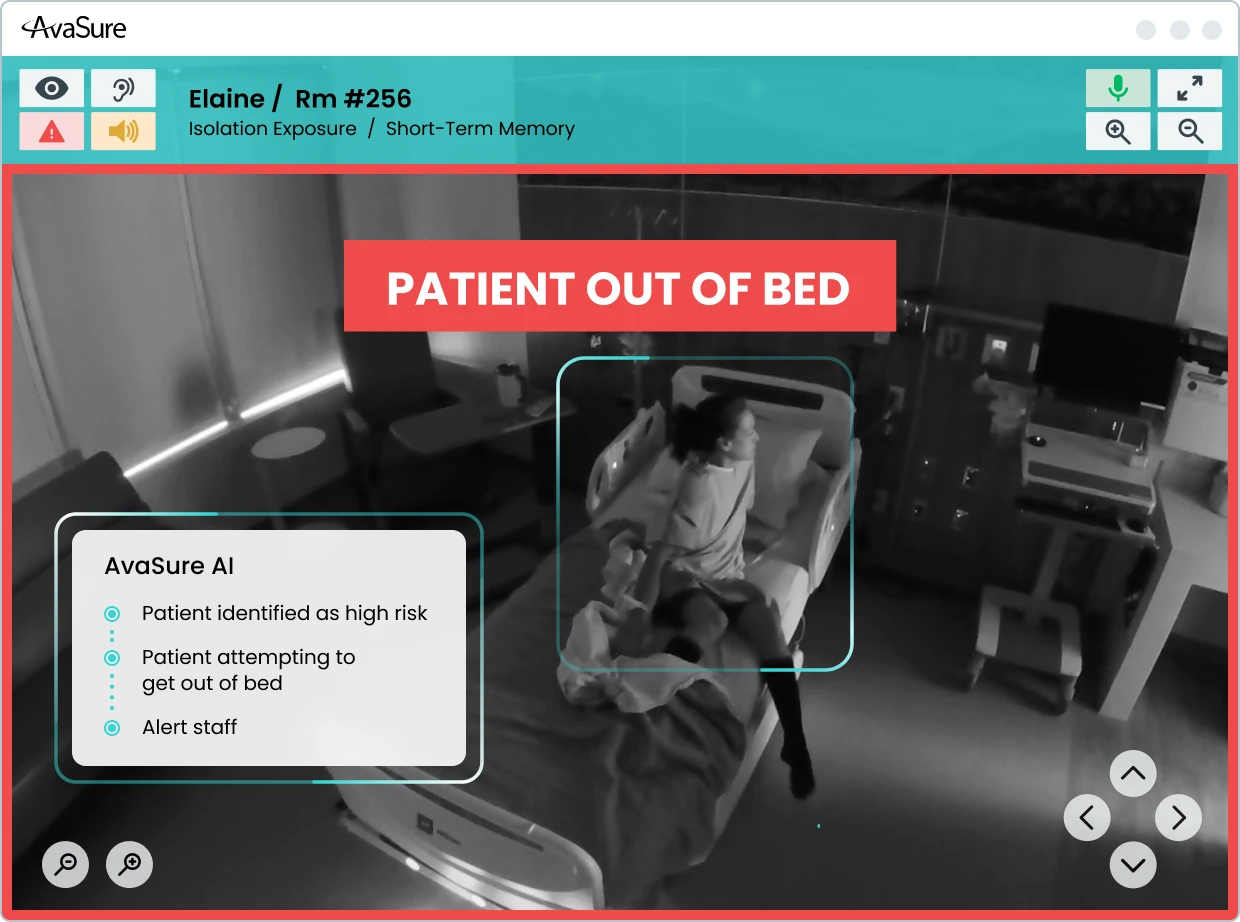
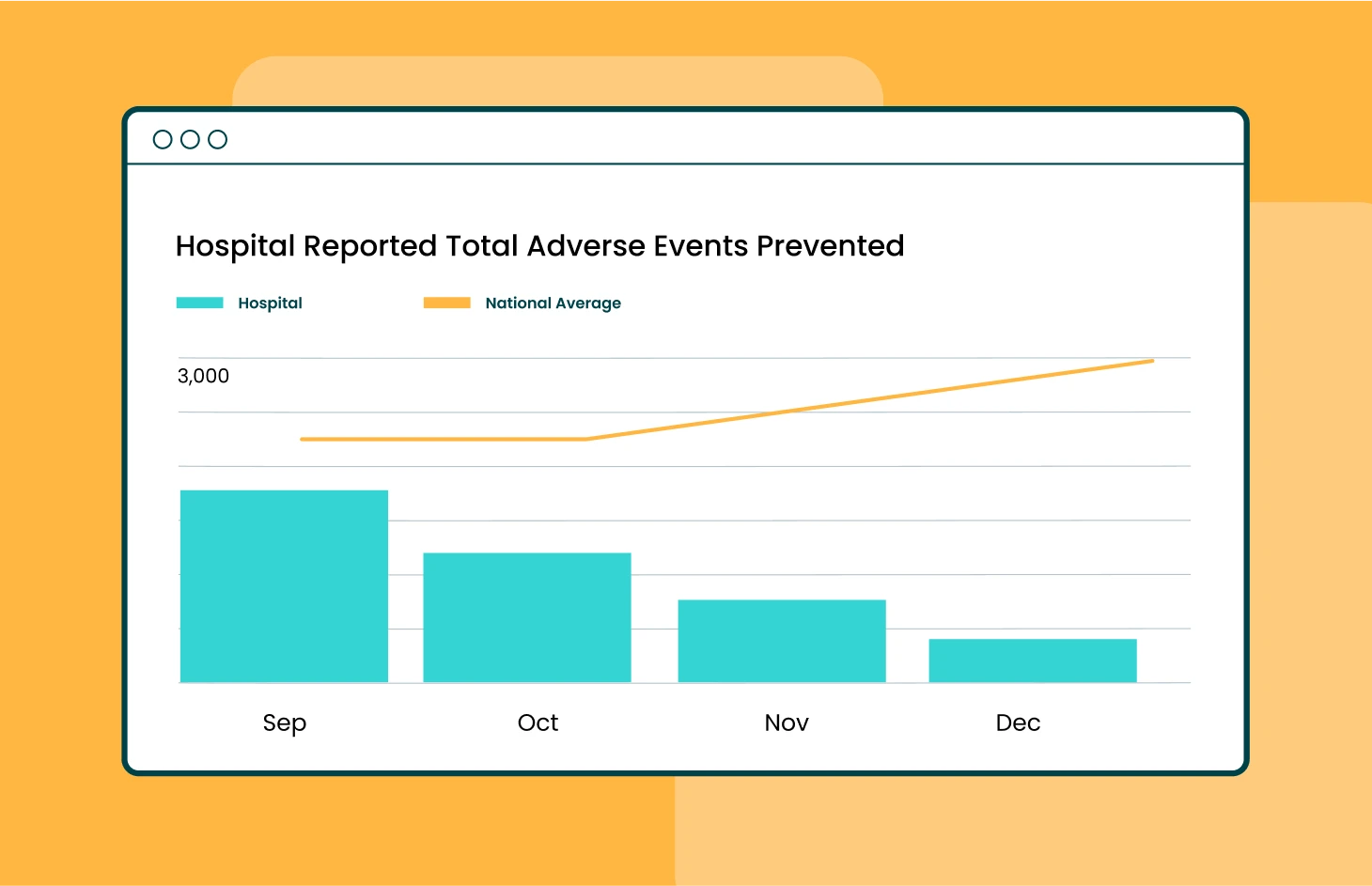
Both UCHealth and HMH began their inpatient virtual care programs with virtual sitting. The program was focused on reducing labor costs associated with 1:1 sitters and preventing patient falls. Virtual sitting is a mainstream nursing intervention proven to help facilities replace an average of 70% of 1:1 sitters while reducing falls rates by up to 60%. UCHealth has saved $9M in labor costs with virtual sitting achieving up to 6x ROI. Facilities can utilize these labor savings to help fund the investment in a virtual care device for every patient room.
Pilot sticking point: sufficient infrastructure & technology
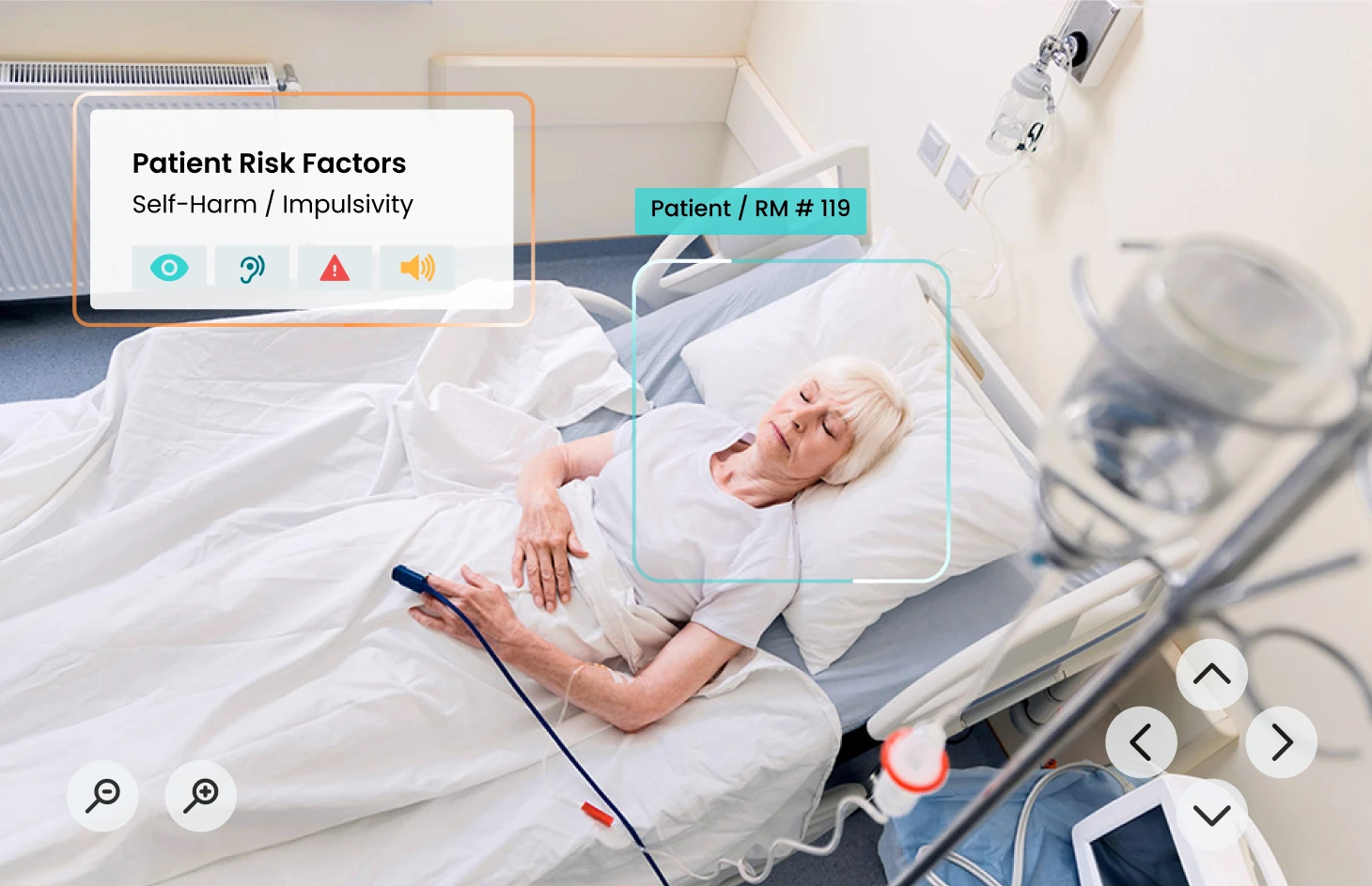
Medical quality audio and video devices are fundamental to enable virtual care workflows. Many pilots rely on mobile carts or tablets as a small proof of concept. However, this makes it challenging to scale as it creates additional workflow challenges that impact program success. Because of this, both UCHealth and HMH now standardize patient rooms with a device included and would recommend the same to anyone considering full-scale virtual nursing. This doesn’t mean you always need to add an additional vendor to your portfolio, as this can be a pain point for IT leaders constantly tasked with vendor consolidation.
Their recommendation: Consider your current technology stack.
You may currently have a vendor in your hospital – like your EHR or virtual sitting provider – that can scale into virtual nursing. This can help to get more ROI out of an investment you’re already making. However, be sure they’re equipped to support you. When selecting a virtual nursing technology vendor, consider the following points:
- Platform ease of use: Be sure to select a vendor with a platform that supports multiple clinical use cases and is easy for nurses to use.
- Support: There is a lot of clinical change & workflow management that comes with implementing a change to the care model, so select a vendor with expertise who will partner with your clinical teams throughout this process. IT teams also have a lot on their plates and shouldn’t be overburdened with implementing a new platform. Consider a vendor who provides robust technical and project management 24/7 support– not just at the time of deployment, but throughout the partnership.
- Demonstrated outcomes: When technology advances, new vendors flood the market. In the clinical space, it’s more important than ever to select a partner with demonstrated experience in delivering outcomes for our patients.
Benefits of a fully integrated virtual nursing program
The promise of virtual care is to create a more sustainable, patient-centered healthcare system that leverages technology to deliver high-quality care anytime, anywhere with greater precision and efficiency. With virtual care workflows as a standard part of care delivery, facilities can meet the evolving needs of both patients & healthcare providers by expanding access to care, improving patient experience, reducing caregiver workload, and increasing the efficiency and scalability of staffing. The path to virtual care maturity requires more than just investing in new technology – it also requires organizational alignment, tight change management processes, and buy-in at all levels of the organization. Adopting an intelligent platform that seamlessly blends remote and in-person care with AI-powered virtual nursing is a critical step towards accelerating virtual care maturity.
Learn more about the AvaSure Platform’s ability to support your virtual nursing growth.
Resources
1 Joslin Insight Virtual Care Insight Study October 2024