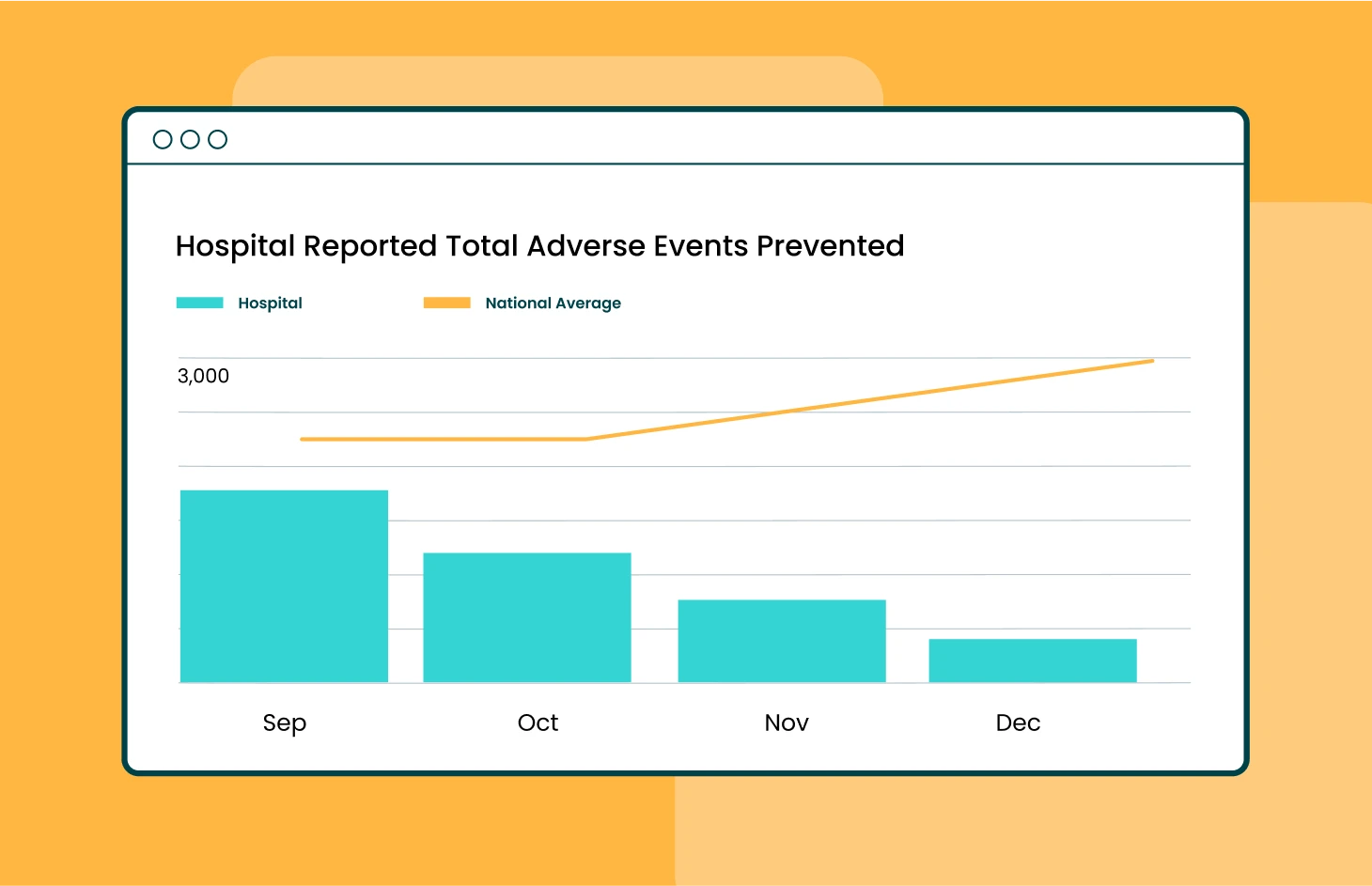
AvaSure Analytics helps providers benchmark virtual care program performance against 800+ hospitals
BELMONT, Mich., [April 8, 2024] — On the heels of its breakthrough innovation with the AvaSure Episodic solution that allows hospitals to transform their virtual care model, AvaSure, has announced significant enhancements to its industry-leading analytics portal that further advances its AI-powered Intelligent Virtual Care platform. The AvaSure Analytics™ portal has been revamped with Microsoft PowerBI tools that enable healthcare providers to conduct deep analysis of critical metrics. As the only comparative database of its kind, AvaSure enables benchmarking an organization’s virtual care program performance against more than 800 hospitals nationwide, including a wide range of sizes and types, to drive care quality improvements and return on investment.
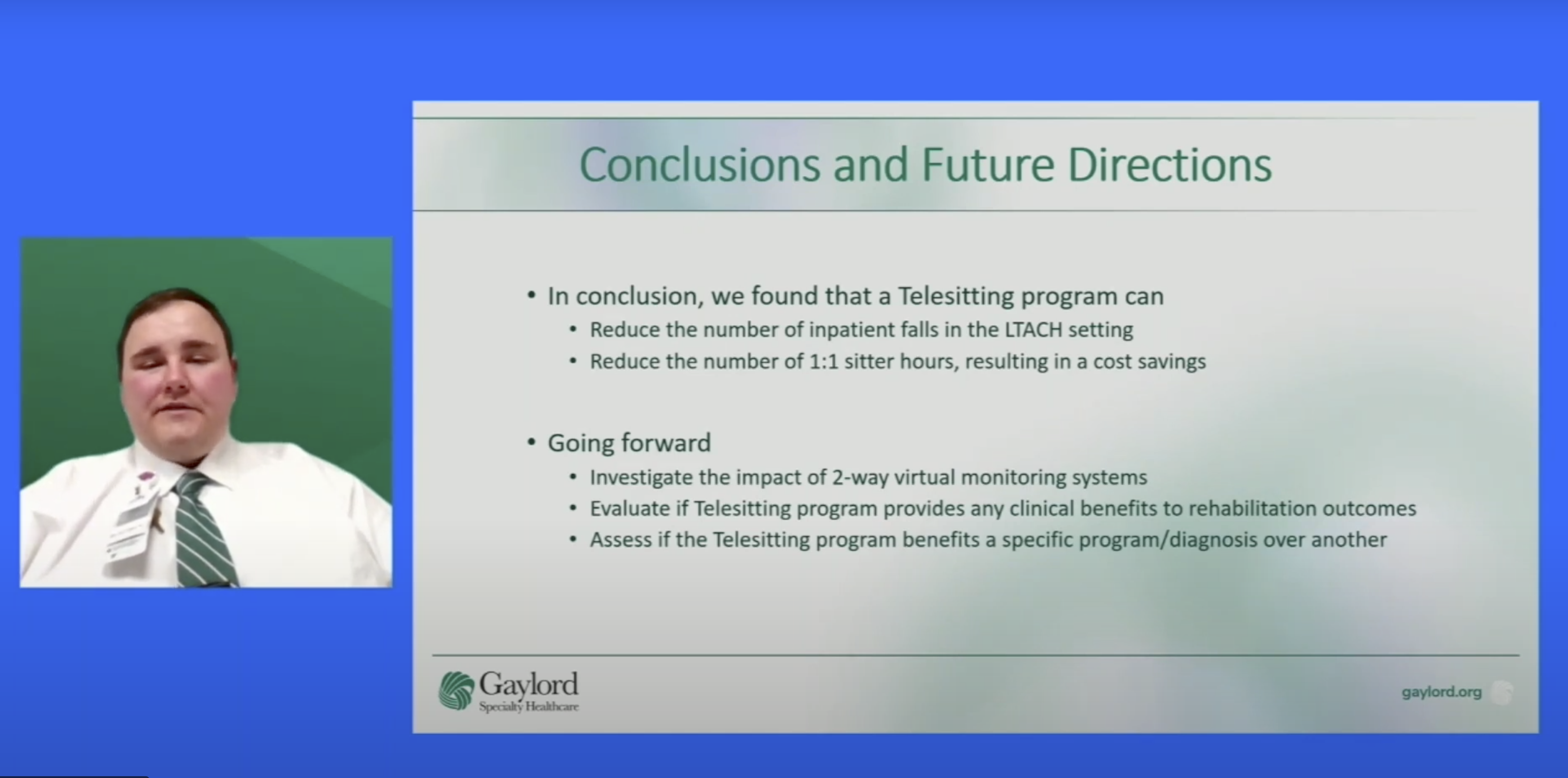
“The AvaSure platform has logged over 145 million hours monitoring nearly 2 million patients across the country, consistently delivering program results that improve patient safety while reducing costs,” said Adam McMullin, CEO of AvaSure. “In addition to delivering measurable labor cost savings by reducing the need for 1:1 sitters by 75%, AvaSure gives hospitals actionable insights based on their own data to further reduce the risk of falls, elopement, workplace violence, and other events. Plus, it allows them to assess the health of their virtual care program by comparing their performance against similar organizations, such as academic medical centers or pediatric hospitals, to track performance against relevant targets.”
Amid persistent staffing shortages and rising pressure to control costs, virtual care has become essential for hospitals looking to adapt. The AvaSure platform enables organizations to seamlessly blend remote and in-person treatment at scale, leveraging AI to use resources more efficiently, respond faster to patient needs, and let clinical teams focus on the work they love. With insightful analytics, healthcare providers gain:
- Actionable Intelligence: With clear insights into labor cost savings, patient demographics, utilization, alarm rates, staff interventions, adverse events prevented and more, organizations can identify and target areas for improvement by care unit and staff member.
- Clear Results: Straightforward visualizations make it easy to equip leadership to communicate program highlights, ROI, and successes.
- Macro to Micro Analysis: Users can view data at the program level and easily drill down into data for care units and individual virtual safety attendants for a granular understanding of performance and opportunities for data-driven intervention strategies.
- Comparative Advantage: Organizations can view benchmarks by the national average and by organization type (e.g., academic medical centers, Magnet®-designated hospitals, Veterans Administration, rehabilitation facilities, critical access hospitals, etc.) to see how they stack up.
“With such straightforward, intuitive access to advanced analytics, the AvaSure platform helps our clients take their virtual care programs to the next level,” said Lisbeth Votruba, MSN, RN, AvaSure’s chief clinical officer. “It’s never been easier for our clients to quantify the value they are receiving, based on both their own metrics and against similar organizations. The latest analytics portal release is an investment in AvaSure’s virtual care platform that demonstrates our commitment to innovation and delighting our customers. By partnering with AvaSure, our customers can be sure that we are going to continue to push the envelope with the latest technology and develop solutions that delight stakeholders across the organization – clinical, IT, and finance.”
The AvaSure Intelligent Virtual Care platform gives organizations flexibility in the use of virtual care solutions that reduce labor costs while ensuring high-quality patient care. Clinicians can admit and discharge patients, engage with them bedside, and monitor them remotely at scale no matter where they are, relieving the onsite team and seamlessly integrating in-person and virtual workflows. AvaSure continuously innovates in the virtual care space while demonstrating a proven record of clinical outcomes with AI-powered continuous monitoring, episodic care, and analytics that help to drive real results.
To learn more about AvaSure analytics, click here or stop by AvaSure’s AONL booth #1112 in New Orleans, April 8-11.
About AvaSure
AvaSure® is an intelligent virtual care platform that healthcare providers use to engage with patients, optimize staffing, and seamlessly blend remote and in-person care at scale. The platform deploys AI-powered virtual sitting and virtual nursing solutions, meets the highest enterprise IT standards, integrates seamlessly with technology partners, and drives measurable outcomes. AvaSure consistently delivers a 6x ROI and has been recognized by KLAS Research as the #1 solution for reducing the cost of care. With a team of 15% nurses, AvaSure is a trusted partner of 1,100+ hospitals with experience in over 5,000 deployments.
Media Contact:
Marcia Rhodes, Amendola Communications
mrhodes@acmarketingpr.com