On July 30th, 2020, as hospitalizations from COVID-19 were hitting new peaks across the country, Memorial Hermann Health System initiated a pilot virtual nursing program at 3 of its hospitals in Texas during its COVID-19 hospitalization surge.
ICUs at Memorial Hermann have large windows that allow nurses to monitor and check-in on patients without physically entering the room. As patients filled hospital beds outside these ICU locations, nurses had to physically enter rooms in full personal protective equipment (PPE) to periodically check in on the critically ill.
The program utilized mobile monitoring devices in rooms so nurses could monitor patients virtually, and soon the virtual program covered 14 ICUs during the summer surge through September. The program was designed to maximize shift efficiency, protect staff and patients from COVID exposure, and centralize protocols based on nursing qualifications.
As the COVID-19 delta variant spread, experienced critical care nurses were sent to a central video monitoring station that managed the health system’s 100 mobile monitoring devices, which allowed communication between less experienced staff to effectively monitor and care for COVID patients in the 2 subsequent surges that followed.
The system also allowed nurses at Memorial Hermann to safely and effectively monitor up to 8 patients from remote (at-home) locations if needed.
Memorial Hermann’s protocols included revamping its staff and nurse practices to accommodate for the high demand created by COVID-19 hospitalization surges and ongoing workforce shortages.
“We also in the future could use [the virtual program] for nurses who may not be physically able to work more than 3 shifts,” said Director of Hospital Information Systems at Memorial Hermann Scott Shaver, MSN and registered nurse. “I have full disclosure, I guarantee you if I was a nurse on the floor right now, I would do 3 shifts and that would be it. I am too old to do more than that.
My body doesn’t work that way [anymore]. But I can guarantee you that I can do 3 shifts in the ER and then do a shift at home using this. I could definitely do that. And so we actually have that availability as well not just for COVID but for really anything in the future. This can be applied to really anything that we can think of in the future where we can use virtual nursing to take care of patients.”
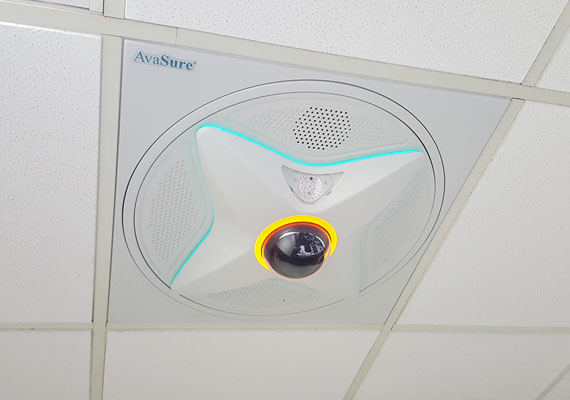
The company AvaSure provided the virtual nursing platform used by Memorial Hermann. The company sells evidence-based virtual care solutions, an innovative set of software and hardware aimed at inpatient telehealth care and utilized in nearly 1,000 hospitals across North America.
Juliet Aninye, a VA North Texas Health Care System nurse and LVN Lead for AvaSure’s TeleSitter® Program, was the winner of the Department of Veterans Affairs (VA) 2022 Secretary’s Award for Excellence in Nursing and Advancement of Nursing Programs.
The AvaSure TeleSitter® solution allows one trained hospital employee to monitor up to 16 patients simultaneously, preventing not only falls but elopement, violence against caregivers, and other adverse events.
“The bedside nurse will select which patients are most at risk for some kind of adverse events,” said Lisbeth Votruba, Chief Clinical Innovation Officer at AvaSure and herself a registered nurse. “[Falling] is a very common one. A frail elderly person who’s disoriented in a hospital setting—if they fall it can be really catastrophic. Those types of patients or a traumatic brain injury patient who’s impulsive and aggressive … or a patient who is in isolation with COVID, is delirious, their oxygen level is dropping, they’ve got to keep a mask on and they keep pulling it off. [It is important] to have the ability to monitor those higher risk patients, which is about 10% of the [in-patient] setting.”
Votruba said the virtual nursing models that have emerged improve efficiencies in patient admission and discharge, virtual preceptor mentoring, and critical care support that leverages nursing expertise across a health system in a centralized manner.
AvaSure’s video platforms that enable physicians and other clinicians to have instant telehealth check-ins with patients and their families are part of a $12 billion global telehealth market that exploded in growth during the pandemic.
Texas plans to invest $600 million over the next several years to expand broadband statewide and improve telehealth access for the 2nd largest rural population in the US. Nearly 2.8 million Texas households, or 7 million people, lack broadband access, according to the US Census Bureau.
According to the Texas Rural Health Association and Rural Health Hub, there are 64 counties in the state without a hospital, 25 counties without a physician, and 75% of counties are designated as Health Professional Shortage Areas (HPSA).
Virtual nursing advocates say the shortage of trained health care professionals in rural areas was an existing problem that was exacerbated by the pandemic and highlighted the state’s current health care system’s inability to reach these vulnerable communities.
The University of Texas Medical Branch (UTMB) School of Nursing will be launching a nursing certificate program in January of 2023 that aims to improve care for patients in rural areas where there are not enough professionals to care for these communities.
“For telehealth to be a widely adopted solution across Texas, providers need resources, education, and support to eliminate barriers and successfully implement telehealth tools into modern health care practice,” said Dr. Kristen Starnes-Ott, Vice Dean for Academic Affairs and Professor at UTMB School of Nursing.
She pointed out that many health care institutions shifted to a telehealth model as an emergency measure when the pandemic began, but much of it was done without adequate training.
With proper preparation, training, and implementation, she said that telehealth has great potential to help Texans receive needed care in areas with a shortage of providers.
Source: Boram, K (August 1, 2022). “Virtual nurse emerged as solution workforce shortage in Texas during pandemic surges”. State of Reform Texas