The Comprehensive Guide: How Can AI Be Used in Healthcare and Patient Care?
Technology
January 8, 2026
In recent history, no technology has so quickly penetrated the cultural zeitgeist as artificial intelligence (AI). At an ever-increasing pace, AI is being hailed as a transformative force capable of revolutionizing industries worldwide, and healthcare is no exception. Companies across the globe are racing to utilize AI to automate, simplify, and rationalize manual tasks across every sector, recognizing its potential to solve some of the most persistent, existential challenges facing modern healthcare systems.
For years, healthcare has grappled with tremendous cost pressure, chronic staffing shortages, and an overwhelming administrative burden contributing to high rates of clinician burnout. Hospitals have focused on utilizing technology to drive significant change through the digitization of documentation, consolidation of health systems, and the virtualization of traditional care models. However, often these tools – while helpful -have not delivered the seamless simplicity, actionable insights, or scale necessary to alleviate the core pressures.
The integration of AI, particularly into technologies like intelligent virtual care platforms, represents a critical shift. It moves us beyond mere digitization to intelligent automation. This guide delves deeply into the capabilities, benefits, challenges, and practical steps necessary for healthcare organizations to effectively harness the power of AI, transforming it from a passing technology trend into a reliable foundation for the future of patient care.
The Core Technologies Driving AI in Healthcare
The umbrella term “Artificial Intelligence” encompasses several distinct technologies, each with unique applications in a clinical setting. To understand how AI can reshape patient care, it is essential to explore these core components in depth.
What is Machine Learning (ML) and Deep Learning?: The Engine of Modern AI
Machine Learning is a subset of AI where systems learn from data, identify patterns, and make decisions with minimal human intervention. Deep Learning, a more advanced form of ML, utilizes artificial neural networks with multiple layers to process complex data, like medical imaging, genomic sequences, or patient physiological data, allowing for highly sophisticated pattern recognition.
Real-World Application: ML models are primarily used in diagnostics and risk stratification. For example, Deep Learning algorithms can be trained on millions of historical electrocardiograms (ECGs) to detect subtle, early signs of atrial fibrillation or myocardial infarction that a human eye might miss. Similarly, in genomics, ML helps identify genetic markers that predispose a patient to certain diseases, paving the way for truly personalized medicine.
What is Natural Language Processing (NLP)?: Transforming Unstructured Data
Healthcare data is notoriously messy. A vast majority of critical patient information – physician notes, discharge summaries, radiology reports, and dictated records – is locked away in unstructured text formats. Natural Language Processing (NLP) is the branch of AI that enables computers to understand, interpret, and generate human language.
In-Depth Use Cases:
- Clinical Documentation: NLP converts free text or speech into structured data, automatically populating electronic health records (EHRs). This drastically reduces the time clinicians spend on administrative tasks.
- Sepsis Detection: Advanced NLP algorithms can scan unstructured notes in the EHR, looking for phrases like “patient looks pale,” “fever spiking,” or “lactic acid elevated,” and combine this with structured data to generate an early warning score for sepsis, often hours before traditional systems would flag the risk.
- Information Retrieval: NLP allows researchers and clinicians to query massive datasets of patient records, finding patterns in treatment efficacy and outcomes that would be impossible to manually extract.
What is Conversational AI and Virtual Assistants?: Bridging the Communication Gap
Conversational AI uses a combination of NLP, machine learning, and dialogue management to enable human-like interactions. In healthcare, this manifests as chatbots, virtual assistants, and intelligent patient portals.
Patient-Facing Applications:
- Triage and Scheduling: AI chatbots can handle initial patient queries, symptoms assessments, and guide patients to the appropriate level of care, or automatically schedule appointments, significantly reducing the workload on call centers.
- Patient Education and Support: Post-discharge, AI can send automated, personalized check-ins and educational content tailored to the patient’s specific condition, ensuring adherence to recovery plans and monitoring for red-flag symptoms.
- Medication Reminders: Virtual assistants can provide timely reminders about medication adherence, which is crucial for managing chronic diseases.
Why is Predictive Analytics Important? Forecasting Health Outcomes
Predictive analytics mines vast amounts of aggregated data, including patient history, real-time physiological metrics, environmental factors, and demographic information to plug into algorithms that project future events or risks.
Key Applications in Risk Mitigation:
- Readmission Risk: Hospitals use predictive models to flag patients at high risk of readmission within 30 or 90 days of discharge, allowing care coordinators to intervene proactively with resources, patient education, or follow-up appointments.
- Sepsis and Cardiac Arrest: By continuously analyzing streaming patient data from monitors and EHRs, predictive analytics can generate real-time risk scores, giving care teams precious hours to intervene before a life-threatening event occurs.
- Population Health: For public health, predictive models forecast disease outbreaks, hospital capacity needs, and resource allocation requirements during crises like pandemics.
What is Computer Vision and AI-Powered Imaging?: Enhancing Diagnostics and Safety
Computer Vision (CV) is the technology that enables AI systems to derive meaningful information from digital images, video, and other visual inputs. Its application in healthcare is rapidly expanding from the laboratory to the bedside.
In-Depth Use Cases:
- AI-Powered Imaging Diagnostics: CV algorithms are trained to analyze medical images (X-rays, CT scans, MRIs, pathology slides) to detect subtle anomalies that may indicate early-stage disease. A critical real-world example is the use of AI tools to rapidly identify pulmonary nodules in CT scans or to flag microcalcifications in mammograms, enabling earlier detection and treatment of lung and breast cancer.
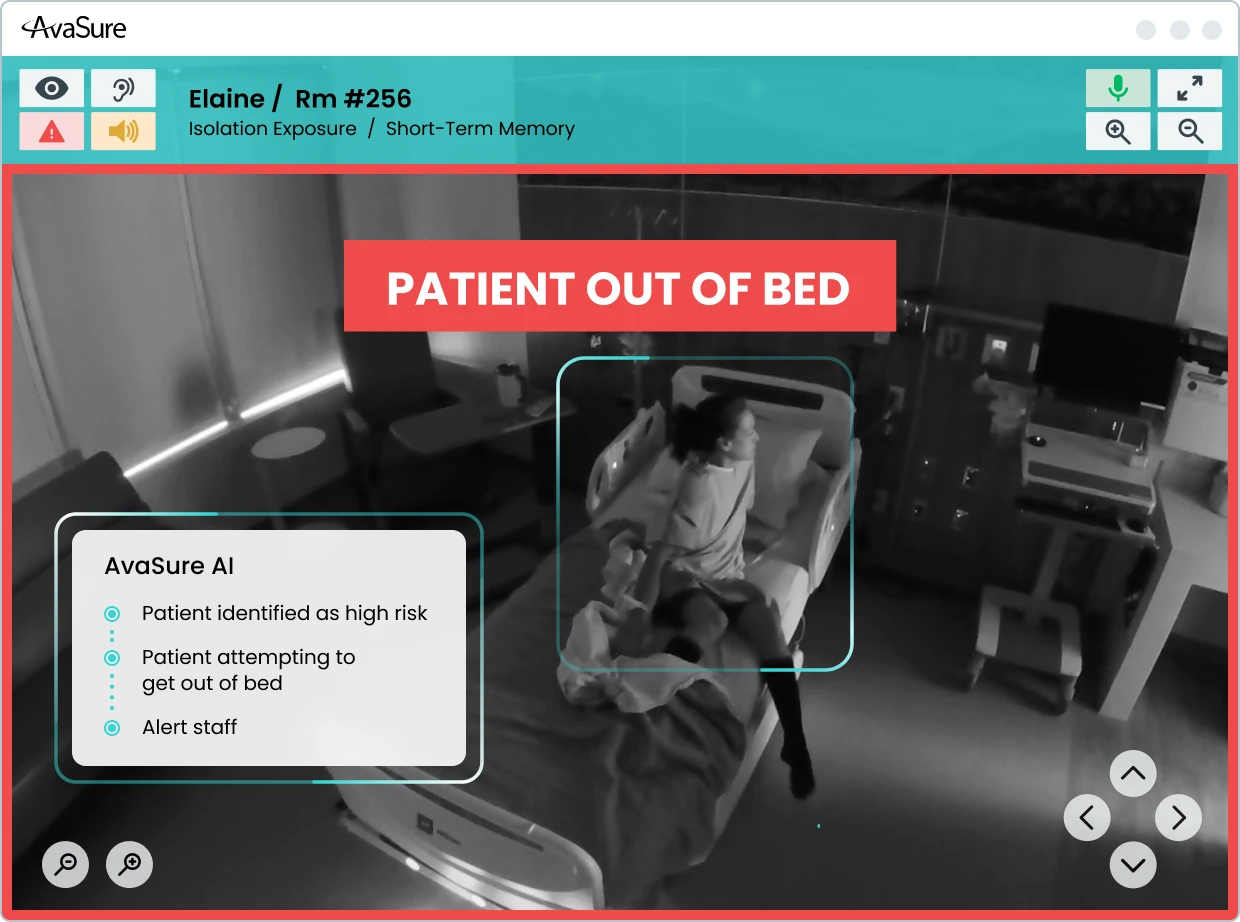
- Patient Safety Observation: At the bedside, sophisticated CV systems embedded in virtual care devices like the AvaSure platform monitor patient movement in real-time. These systems can identify high-risk behaviors, such as a patient attempting to climb out of bed or a visitor violating isolation protocols, and issue immediate, actionable alerts to a remote observer. This proactive monitoring dramatically reduces the occurrence of Never Events like patient falls and the development of hospital-acquired pressure injuries (HAPIs) by intervening before injury occurs.
Why Ambient Listening is Important: Alleviating Clinician Burden
Ambient listening technology uses microphones to capture conversations, typically between a patient and a clinician, and then employs NLP to transcribe and structure the content. This is distinct from NLP in that it is designed for a live, real-time clinical encounter.
Use Case: Clinical Scribing: The primary application is to automatically draft clinical notes. Instead of typing into the EHR during or immediately after an encounter, the clinician can focus entirely on the patient. The AI listens, captures key phrases like medical terms, diagnoses, orders, and action items, and populates the patient’s chart, saving hours of administrative time and directly combating clinician burnout.
AI’s Direct Impact: What are the Benefits of AI for Patients and the Patient Experience?
While much of the early AI focus centered on efficiency and cost savings for hospitals, the most profound impact of this technology is on the patients themselves: improving safety, quality of life, and the overall healthcare experience.
Personalized Medicine and Treatment Planning
AI’s ability to process complex, multi-modal data is the backbone of precision medicine. By integrating a patient’s genomic data, electronic health record, lifestyle information, and even wearable device data, AI can create a highly detailed, predictive portrait of their health. This allows physicians to:
- Tailor Drug Dosing: Determine the exact medication and dosage that will be most effective for a patient based on their genetic makeup, minimizing adverse reactions.
- Optimize Treatment Paths: Predict how a patient’s cancer will respond to specific chemotherapy or radiation protocols, adjusting the plan in real-time based on AI-driven feedback loops.
Enhanced Patient Experiences through Virtual Assistants
A hospital stay can be confusing and stressful. AI-powered virtual assistants are beginning to serve as in-room digital concierges, empowering patients and reducing the need for non-clinical nursing interruptions.
- Simple Request Fulfillment: Patients can use voice commands or a tablet interface to request essential, non-urgent services, such as a blanket, a meal menu, or adjustment of room temperature, which are then automatically routed to the appropriate department.
- Information Access: The virtual assistant can answer common questions about the hospital facility, discharge procedures, or medication schedules, providing instant information and reducing the burden on clinical staff.
Personalized Patient Education and Engagement
General patient handouts often fail to resonate. AI can dynamically generate educational content that is tailored to a patient’s:
- Health Literacy Level: Adjusting complexity and vocabulary to ensure understanding.
- Specific Context: Focusing education on the exact medications or procedures the patient has undergone.
- Preferred Language: Offering information in native languages, improving comprehension and adherence.
How Do You Expand Access with AI in Telemedicine Services?
AI is fundamentally changing the delivery model of telemedicine, allowing for remote care to be more sophisticated and scalable.
- Virtual Nursing Support: Virtual Nursing programs leverage remote clinicians to assist with tasks like admissions, discharges, medication reconciliation, and patient education. AI enhances this by identifying which patients require an immediate virtual check-in based on real-time risk scores and physiological data, allowing remote nurses to prioritize their attention to where it is needed most.
- Remote Diagnostics: AI-enabled tools allow general practitioners in rural settings to upload specialized images or data (e.g., dermatological pictures or retinal scans) that are instantly analyzed by AI for preliminary diagnosis before being sent to an off-site specialist for final review.
Navigating the Complexities: What are the Challenges and Ethical Considerations of AI?
The transformative potential of AI is matched by significant challenges, particularly concerning ethics, data, and regulatory oversight. Ignoring these issues risks undermining the very trust AI is intended to build.
The Critical Need for Trust and Transparency (Explainability/XAI)
One of the most persistent issues in AI is the “black box” problem. Many sophisticated deep learning models are so complex that even their designers struggle to articulate why a particular decision was made. In healthcare, where decisions can be life-altering, this lack of data interpretability is unacceptable.
- Explainable AI (XAI): The imperative is to develop XAI tools that can not only provide a diagnosis or risk score but also show the underlying data and logic used to arrive at that conclusion. Clinicians need confidence in the tool, and patients deserve to know why a treatment path was recommended.
- Validation of AI Models: Before deployment, every AI model must undergo rigorous validation using external, real-world data sets to ensure it performs accurately and consistently across diverse patient populations.
Validation, Verification, and the Risk of Hallucinations
AI systems, particularly large language models (LLMs) used in conversational AI, are susceptible to hallucinations – generating plausible-sounding but factually incorrect information. In a clinical context, a hallucination could lead to a catastrophic medical error.
- Verification: Implementing AI systems requires robust verification loops, ensuring that AI-generated clinical notes, suggested diagnoses, or treatment plans are always reviewed and approved by a qualified human clinician before execution.
- Model Drift: Healthcare systems must continuously monitor AI performance because models can “drift” over time as new patient data or clinical protocols emerge, making the original training data less relevant.
Addressing Bias and Ensuring Ethical AI Decisions
AI is only as objective as the data it is trained on. If a training dataset over-represents one demographic (e.g., white, male, high-income patients) and under-represents another (e.g., minority, low-income, geriatric patients), the resulting AI model will be inherently biased.
- Health Equity: Deploying biased AI systems can exacerbate existing health inequities by systematically under-diagnosing, over-diagnosing, or recommending suboptimal treatment for under-represented groups.
- Ethical Implications of AI Decisions: Organizations must establish clear guidelines for when an AI’s recommendation can be overridden, who is accountable when an AI decision leads to an adverse event, and how the system promotes fairness and equity in access to care.
Regulatory Hurdles and Data Governance
The deployment of AI tools that actively influence diagnosis and treatment requires stringent regulatory approval, typically from the FDA. Unlike a software update, a change to the AI model itself may require a new review. Furthermore, data governance is paramount:
- HIPAA Compliance: All healthcare AI must adhere to strict privacy regulations (like HIPAA in the US) regarding the collection, storage, and processing of protected health information (PHI).
- Data Security: AI requires massive amounts of data, making the security of these large repositories a top concern to prevent breaches and maintain patient trust.
A Practical Roadmap: How Do You Implement AI in Healthcare Organizations?
The adoption of AI should not be a scramble for the latest gadget, but a deliberate, strategic investment. Healthcare organizations need a practical, stepwise approach to implementation to maximize return on investment and clinical benefit.
Stepwise Adoption: Aligning Needs and Goals
Paul White, Distinguished AI Engineer for AvaSure reminds us, “It is important to take a stepwise approach to adoption. Many companies are rolling out AI solutions geared towards creating new efficiencies or solving different issues within the hospital setting. Therefore, the first step should be identifying companies that are building AI solutions that address most crucial areas of need.”
The initial phase must focus on organizational readiness and strategic alignment:
- Assess Readiness: Evaluate existing IT infrastructure, data governance protocols, and the quality of historical data. AI relies on clean, accessible data.
- Identify Crucial Areas of Need: Do not implement AI just for the sake of it. Where are the organization’s most acute pain points? Is it staff retention, patient falls, sepsis mortality, or long wait times? The AI solution must directly address a high-priority problem.
- Define Success Metrics: Clearly define what success looks like before implementation (e.g., “Reduce patient falls by 50% in the first year,” or “Decrease time spent on charting by 2 hours per nurse per shift”).
Prioritizing Use Cases for Maximum Impact
Once organizational needs are identified, organizations can align those needs with the AI technology that offers the most immediate, tangible solution.
Example 1: Addressing Clinician Burnout
- Need: Excessive administrative burden, high EHR time.
- AI Solution: Leveraging AI Clinical Documentation/Scribing solutions (Ambient Listening/NLP) is a great choice for alleviating administrative burden and allowing clinicians to refocus on patient care.
Example Two: Mitigating Never Events
- Need: High incidence of falls, Hospital-Acquired Pressure Injuries (HAPIs), Hospital-Acquired Infections (HAIs).
- AI Solution: Partner with Virtual Care companies leveraging computer vision to mitigate the occurrence of these events. AI monitors the patient’s room 24/7, detects high-risk actions (e.g., a patient reaching for a line), and alerts a remote observer before the patient falls, turning reactive care into proactive prevention.
Build, Buy, or Partner?
A critical strategic decision is whether to develop an AI system internally or acquire a solution from an external vendor.
- Build (Internal Development): Requires massive internal investment in data scientists, ML engineers, and clean training data. This is typically only feasible for the largest health systems with deep research capabilities.
- Buy (Vendor Solution): The most common path. Healthcare organizations can purchase validated, ready-to-deploy solutions. Paul White adds, “It is crucial to understand and align with a vendor whose ethos matches your own.” Look for vendors who demonstrate a commitment to:
- Clinical Validation: Providing proof of concept and third-party validation studies.
- Seamless Integration: Ensuring the AI solution integrates smoothly with existing EHRs and virtual care infrastructure.
- Ethical AI: Showing commitment to transparency, minimizing bias, and data security.
Change Management and Clinician Buy-in
No matter how powerful the technology, AI implementation will fail without clinician support. The fear that “AI will replace my job” must be addressed head-on.
- Focus on Augmentation, not Replacement: Position AI as a “co-pilot” or intelligent assistant that removes tedious tasks, enhances diagnostic capability, and reduces cognitive load, allowing clinicians to practice at the top of their license.
- Training and Workflow Integration: Training should focus less on the technology of AI and more on how it seamlessly fits into and improves the existing clinical workflow.
Looking Ahead: What are the Future Trends of AI in Healthcare?
The integration of AI into healthcare is not an end point, but the beginning of a new era of medical practice. The next decade promises even more radical transformation.
Deeper Integration of Virtual and In-Person Care
Anticipated technological advancements will blur the lines between virtual and physical care:
- Ubiquitous Sensors: Low-cost, non-invasive sensors (wearables, smart textiles, in-room monitoring) will feed continuous, high-fidelity physiological data into AI systems.
- Closed-Loop Automation: AI will move beyond alerts to initiating automated actionsfor example, automatically adjusting IV pump rates based on real-time blood pressure data, or using an in-room virtual care platform to deliver a two-minute therapeutic intervention immediately after a patient is flagged as high-anxiety.
The Era of Tech-Healthcare Collaborations
The future will be defined by strategic partnerships between leading technology firms (Google, Microsoft, NVIDIA, etc.) and pioneering healthcare organizations. These collaborations are essential because tech companies bring computational power and AI expertise, while healthcare partners bring critical, proprietary clinical data and workflow knowledge. This synergy will accelerate the development of lifesaving, regulated AI solutions.
AI as a True Co-Pilot for Healthcare Delivery
In the long term, AI will function as a true co-pilot for every member of the care team:
- For Radiologists: AI systems will triage scans, flagging critical cases and providing initial measurements, allowing the human expert to focus their attention and time on complex diagnoses.
- For Surgeons: AI will assist in pre-operative planning, intra-operative guidance using computer vision for precision, and robotic assistance, leading to safer, more reproducible outcomes.
- For Nurses: AI-enabled virtual care will handle many of the repetitive safety checks and administrative tasks, allowing nurses to spend their time at the bedside engaging in therapeutic communication, complex problem-solving, and providing the essential human touch that AI can never replace.
Conclusion: Fact vs. Fiction
AI is no longer a futuristic concept; it is a present-day reality that is already driving efficiency and saving lives. The technologies, from Machine Learning diagnostics to Computer Vision patient safety platforms, are primed for widespread adoption. By taking a thoughtful, stepwise, and ethically sound approach to implementation, healthcare organizations can ensure that they are not just adopting a new technology, but building a more resilient, efficient, and patient-centric healthcare system for the next generation.
To learn more about the reality of AI adoption in the clinical setting, watch our Webinar featuring Aaron Miri, Senior VP and Chief Digital and Information Officer of Baptist Health and Elizabeth Gunn, VP of Patient Services for Baptist Medical Center South: AI in Healthcare: Fact vs. Fiction
Ready to get started?
Get in touch with an AvaSure representative to learn more about AvaSure's AI-enabled virtual care solutions.