The Importance of Centralized Monitoring in a Health System’s Patient Safety Program
No topics assigned.
December 22, 2022
Key insights and takeaways from successful patient safety programs.

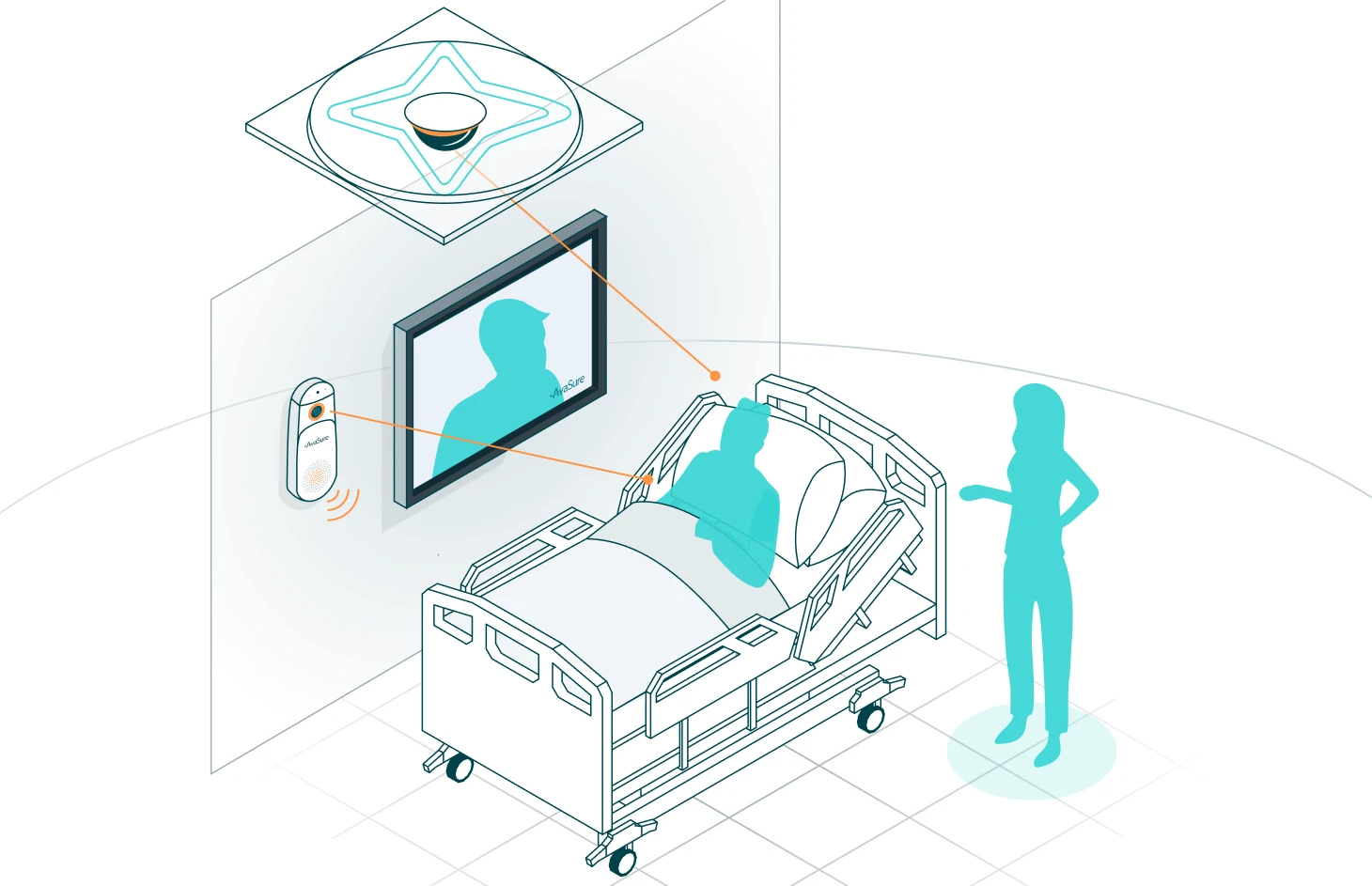
Historically, health systems and hospitals have used ‘patient-sitters’ to provide direct and one-on-one monitoring support to their patients. But this method is expensive and inefficient. Many healthcare systems have identified the importance of a centralized patient safety program for labor optimization and providing value-based care and have scaled to hub and spoke model systems, increasing their coverage through a centralized monitoring model. Read on to learn more on how hub and spoke models are becoming the norm for virtual care.
Streamlining patient care with a hub and spoke model
- When an administrator at Baptist Health Medicine spotted a sitter in full PPE in a room when doing rounds on a COVID floor, she came up with the idea to introduce the TeleSitter® solution. She got the parties from all six campuses as well as the leaders in the fields of executive, nursing, financial leadership, social work, and case management. Within 18 months, the project went from piloting with 16 cameras to centralized, off-site operation covering multiple facilities. Implementation of the centralized system involved 100 team members!
- To make sure that a workforce would be available, Loyola Medicine looked at the location of the hub while monitoring all four time zones. Cost of sitters, fall rates, and present-day costs associated with falls were examined. The estimated number of patients requiring monitoring at each facility was used to decide how many cameras per hospital to install.
- A best practice for budgeting hub & spoke – each facility receiving monitoring in the hub & spoke model pays for 60% of the program. This budget then supports virtual safety attendants (VSAs), regardless of utilization. It’s important to keep the FTE level of virtual safety attendant staff adequate so you can monitor the requested number of patients at any given time. Cox Health uses a similar model to support their patient safety program. In year 1, they reduced the requirement for 30 FTE sitters, saving $1.3M. Since remote hospitals lack sitter reserves, cameras have been helpful in preventing staff from being called away from the floor.
Data collections across health systems
- Many healthcare systems run extremely differently from one another (even when part of the same IDN) and efforts to harmonize data collecting are still a work in progress at many systems. At Baptist Health Medicine, falls have been identified as a core metric to measure results of the TeleSitter system. The system’s fall committee tracks “falls” and “falls with injury” using an incident reporting system. YoY comparisons are made to ensure that as they reduce sitter counts, they see reduction in falls as well. Prior to AvaSure, there was no reliable statistic for tracking sitter impact.
- Sharing data throughout the system can help to garner buy in for your patient safety program. Once a month, Loyola Medicine holds a hub & spoke meeting where data is presented at the hub level, but also broken down by each spoke so that everyone can see their individual results. This makes it easier to benchmark each facilities effectiveness by looking at important indicators such as stat alarm reduction time & utilization. Asking leaders to bring information to the meeting such as falls data (not collected in ORNA®) can help make it a productive time to share other results as well. The dashboard in ORNA helps them be accountable to how VSAs are performing and quantify the value they’re bringing to the hospital. This meeting helps collect results to hold staff accountable and demonstrate program effectiveness to leadership.
Building support: How to get your patient safety programs off the ground
- Facilities have different approaches on staff background required to become a virtual monitor team member; some require entry-level staff to have a general understanding of healthcare. PCTs or CNAs are also great candidates as they have all worked and gained hospital experience. Given medical expertise, the learning curve is lowered, and this can help to build a team of more experienced VSAs to balance out anyone who may be new to the industry.
- To give virtual safety attendants a perspective for what RNs are dealing with, Loyola Medicine implemented “reverse shadowing” with new hires helping to overcome the obstacle of how each side views “what you truly do all day.” Cox Health has specific qualifications they look for in a VSA, including a positive attitude and demeanor to help foster positive interactions with patients. They are hired as an in-person sitter first, and then after 30 days may permanently place them in a VSA role depending on their understanding of the healthcare space intimately and their technological abilities.
- Cox Health prioritizes education for both groups. To keep personnel accountable, discuss the necessity for vocal intervention. If calling the nurse, verbally intervene first to ensure it’s documented. Also, make sure that bedside staff knows when monitors are and are not monitoring the patient to ensure no moment is missed. Education and communication are key to bridging the gap between the two groups and will be a continual work in progress.
- For VSAs to recognize the importance of their position, they must feel connected with patients, family members, and team members in the hospital. A best practice at some facilities is to have a nurse manager or ANM from one of the spokes round at the departments they’re monitoring to help foster relationships with the bedside. Virtual safety attendants are more likely to find success when they have these relationships with the bedside teams they’re supporting. Presenting at nurse leadership meetings across the spoke facilities help identify new and emerging problems and pain points, helping to continue to optimize the focus of your patient safety program.
Build a strong team – Hire, train & retain staff
- Maintaining a strong team is another key to long-term patient safety program success. Having a house-wide partnership council where all nursing staff are welcome to participate to enhance processes can help with this. This council allows participation from virtual monitors, connecting them to the bedside staff and allowing them to develop process changes, introduce initiatives to the whole company, and bounce ideas off different roles. Each unit has a council that any staff member may join as a subset.
- Loyola Medicine has struggled with retention, so they try to get creative and create more flexibility beyond 12-hour shifts when it comes to scheduling, trying to ensure that they get enough rest and adequate breaks but also considering work/life balance expectations of people interested in this role. When hiring, consider their chances for advancement and where they want to go next; many who start as VSAs are then interested in opportunities to apply to CNA programs, etc., providing a talent pipeline for your organization. At Loyola Medicine, this is so common that they are developing a virtual monitor attendant/CNA program so they can perform both roles in a more flexible program.
- Creating a fun and interactive environment has helped multiple facilities keep staff satisfied and retain them long term. Office items such as sit-to-stand desk or stationary exercise equipment can help to break up the day for workers pulling long shifts. Some offices take it further with “fun Friday” including activities like potlucks, PJ parties, karaoke, or a hot chocolate bar. Because the office is not on site at the hospital, their office setting is more accommodating to these types of work activities. It has created such a great culture at Loyola Medicine that there is a waiting list for VSA roles when many other departments are struggling for staff.
- Having a lead virtual safety attendant who isn’t assigned to specific patients can also help when centralized monitoring increases the number of patients being monitored. What is the lead’s role?
- Be the resource relief for team
- Relieve them for breaks & be a second pair of eyes
- Lead the majority of communication with hospital – troubleshooting, tracking down numbers, etc.
- Do all the admissions & discharges into the TeleSitter system so they can focus on patient care
- Balance workloads, manage patient assignments, and manage VSA’s patient mix between “busy” and “less busy” patients, optimizing their efficiency
- Ensure that the virtual safety attendants are doing their work properly by conducting accountability tracking
- The importance of recognition:
- Emailing virtual safety teams and bedside workers with great catches and highlighting the work of the combined teams every few weeks can help to boost moral of the teams and generate buy-in.
- Use team or staff meetings, orientation, or any time in front of facility staff as an opportunity to highlight the work of the patient safety programs/teams.
- Encourage the use of “kudos” in HR systems to celebrate great catches, but overall, make sure both VSAs and nurses see the good they’re doing in keeping patients safe and make them feel like invaluable assets of the team.
Insights and takeaways to get you started
- When getting started, involve more stakeholders than less. Think about departments likes security, biomed, and all nursing units – ensure everyone who may have a hand in the patient safety program has a voice.
- Consider a steering committee to develop and implement required policies and procedures. This steering committee can also help to guide the program, facilitating communication between departments and driving growth over time. Especially when working with pediatrics, behavior health, or higher risk patients, it’s important to collaborate and communicate regularly to keep the patient safety program running smoothly.
- Don’t stop at falls! Many say they started their patient safety programs focusing only on falls, but over time saw value with a number of other use cases and many wish they had expanded sooner to things like:
- Monitoring eating disorder patients
- Accompanying elderly patients who may be suffering from delirium, dementia, or simply loneliness
- Mental health monitoring of low and moderate suicide ideation patients
- NICU monitoring for kidnapping risk
- Monitoring of patients with family members posing a risk to the patient or staff
- Establish bonds with your spokes, including facility leadership and bedside staff. The ones where leaders are engaged with and have a relationship with the TeleSitter teams have better performance than other units.
- Help your staff recognize the delicate balance between keeping an eye on patient safety vs. being big brother. It’s not their focus to judge nursing jobs, i.e., document “not rounding enough” or commenting on nurse performance. This can help drive trust between nursing and VSAs.
- Early involvement in system falls teams, committees, etc. is important. If you don’t make yourself top of mind, people may forget you are there. Getting involved early is key.
Centralized monitoring is a great way for a patient safety program to create efficiency while delivering improved patient outcomes. Virtual safety teams bridge the gap between patients and nurses, being a true part of the team helping to ensure patient safety and improved outcomes. With the staffing shortage continuing to increase, it is more difficult than ever to find patient sitters without further exacerbating staffing challenges. Virtual sitting is proven to be a safe and reliable way to monitor a variety of patients, while reducing labor costs, driving improved patient safety, and quality outcomes. At AvaSure, we have a best-in-class team that helps establish the goals of your health system while maintaining high-reliability, expertise, quality, and safety. To learn more about how we can help you streamline and increase quality patient care, contact us and get a free complimentary on-site assessment.
Watch the recorded session with Loyola Medicine, Baptist Health Medicine, and Cox Health or download the guide for more best practices.
Ready to get started?
Get in touch with an AvaSure representative to learn more about AvaSure's AI-enabled virtual care solutions.